ORIGINAL RESEARCH ARTICLE | https://doi.org/10.5005/jp-journals-10071-23433 |
Impact of Critical Illness on Quality of Life after Intensive Care Unit Discharge
1,4,6Department of Anesthesia, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
2Department of Anesthesia and Critical Care, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India
3Department of Critical Care Medicine, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
5Department of Biostatistics and Health Informatics, Sanjay Gandhi Postgraduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India
Corresponding Author: Ritu Singh, Department of Anesthesia and Critical Care, Indira Gandhi Institute of Medical Sciences, Patna, Bihar, India, Phone: +91 8127395753, e-mail: ritusingh140@gmail.com
How to cite this article Rai R, Singh R, Azim A, et al. Impact of Critical Illness on Quality of Life after Intensive Care Unit Discharge. Indian J Crit Care Med 2020;24(5):299–306.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Objective: To assess the quality of life (QoL) following intensive care unit (ICU) discharge using 6 months’ prospective follow-up and to analyze the risk factors affecting quality-of-life post-discharge.
Design: A prospective observational cohort study. Conducted on adult patients, discharged from ICU after more than 7 days’ stay. Study duration is from January 2017 to October 2018. Patients %3C;18 years, nonconsenting, preexisting neurological illness, and lost to follow-up were excluded. Follow-up was done at 1 and 6 months using the SF-36 questionnaire. The pre-ICU functional status, patient demographics, sequential organ failure assessment (SOFA) score, acute physiology and chronic health evaluation (APACHE II) score, New York Health Evaluation (NYHA) classification, and details of ICU stay were collected.
Results: One hundred patients (M = 60, F = 40) with ICU stay (13.64 ± 3.75 days), days of mechanical ventilation (7.93 ± 3.89 days), admission APACHE II (18.88 ± 4.34) and SOFA (7.73 ± 1.54) scores. Comparison showed physical component summary (PCS) score and mental component summary (MCS) score at pre-ICU were 55.12 and 55.09 which decreased to 39.59 and 35.49 (p < 0.05) at 1 month post-discharge and 47.93 and 37.46 at 6 months. Age, APACHE II, and SOFA scores are the significant factors affecting PCS and MCS. Length of ICU stay and duration of mechanical ventilation did not affect significantly at 6 months. When compared with general population PCS and MCS showed significant deterioration at 1 and 6 months.
Conclusion: Post-ICU discharge patients have significant functional impairment and compromised health-related QoL (HRQoL). Age and severity of illness significantly affects health quality parameters and decline is below the normal data of general population.
Keywords: Acute physiology and chronic health evaluation II, Critical illness, Quality of Life.
INTRODUCTION
Patients admitted in intensive care unit (ICU) with critical illness have a high mortality and morbidity.1 Initially survivor and death were considered the main outcomes after ICU admission.2 With better ICU care, advancement in medical therapies and improved technology, the number of ICU survivors is increasing day by day.3 Despite a reduction in mortality, these survivors frequently experience long-lasting complications of being critically ill.4 These complications can be caused by disease pathophysiology itself, organ dysfunction developed during hospital stay or any dysfunction acquired during the ICU stay and/or prolonged intensive care support of failed organ(s).5 Critical illness and ICU care can influence the wide range of patient outcomes leading to prolonged impairments and morbidity.6 Patients who have recovered from acute illness can have an effect on physical, mental, psychological, and cognitive power after recovery.7 Spectrum of complications can be varied and long-lasting such as impaired pulmonary function, neuromuscular weakness, neuropsychiatric complication, depression, and post-traumatic stress disorder.8,9 To totally evaluate the quality of life (QoL) and health of these patients, objectivity in clinical assessment, laboratory analyzes, and subjective perception of the physical and mental QoL by patients themselves become important.
The aim of this study was to evaluate HRQoL during 6 months of follow-up after discharge from ICU and to analyze the factors that affect the QoL.
MATERIALS AND METHODS
This was a single-center, observational prospective study carried out in an ICU of a tertiary care center. Institutional ethics committee approval (Ref. PGI/BE/306/2016) was taken and written informed consent from patient or next of kin was also taken. This study was conducted between January 2017 and October 2018. Of the 450 admissions, a total of 100 patients met the inclusion criteria. Eligible candidates were adult patients who received more than 7 days of ICU care and got discharged. Patients with ICU stay of less than 7 days, age of less than 18 years or more than 70 years, refusal to participate in the study, not responding to telephonic calls or postal communication, patients discharged without medical advice, those with terminal illness, and patients having prior history of neurological or psychiatric illness were excluded from the study.
Sample Size Calculation
Sample size calculation was based on previous studies on value of physical component summary (PCS) score, assuming the difference in mean PCS as 7.75 (55.12 to 47.34) between pre-ICU status and at 6 months. Taking α error as 0.5 and the power of study as 80%, sample size needed for our study is 75. Hence, we took 100 patients for our study, assuming that 20% will be lost to follow-up per the previous studies.
Data Collection
Comparison of QoL post-ICU discharge was done with the status before the acute illness. For this, patients, relatives, next of kin, or family members residing with the patient were asked to complete a performa (Annexure). Special emphasis was given on QoL of patients before their current acute illness (4-week recall assessment). Questionnaire was based on short form (SF)-36–Item Health Survey. The Medical Outcomes Trust Short Form-36 Version 2 (SF-36) Health Survey was usedto assess HRQoL. It has demonstrated to have acceptability, reliability, and validity in the critically ill patients.8,10 The higher the score, the better the QoL. It is a comprehensive generic 36-item questionnaire based on eight parameters, namely, physical functioning (PF), body pain, role limitations due physical health problems, personal or emotional problems, emotional well-being, social functioning, energy/fatigue, and health perception. Detailed ICU data were recorded which included patient demographics, severity of illness at ICU admission [sequential organ failure assessment (SOFA) and acute physiology and chronic health evaluation (APACHE II)], length of ICU stay, and duration of mechanical ventilation. Few patients who did not turn up to ICU follow-up clinic were followed through telephonic communication. Of the 100 enrolled patients, telephonic follow-up was needed in 20 patients. Data of PCS/mental component summary (MCS) were compared to general population at baseline, 1 month, and 6 months. Normative data of QoL of general population were compared with the European standard as no Indian data were available.11
STATISTICAL ANALYSIS
Normality of the continuous variables was presented using mean ± standard deviation and categorical data in frequency (%). Repeated-measures analysis of variance [(ANOVA) (RMA)] was used to test the mean change in the study variables at baseline, 1 month, and 6 months. If RMA was significant, multiple pairwise comparisons (using Bonferroni method) were used to identify the significant pairs. Error bar graph was used to present the association between ages, ICU stay, mechanical ventilator, APACHE and SOFA, and PCS and MCS. The p value <0.05 was considered as statistically significant. Statistical data analysis was carried out using the software Statistical Package for Social Sciences, version-23 (SPSS-23; IBM, Chicago, USA). Normative data were obtained from quality metric 2009 general population sample of Europe.11
RESULTS
Of the 100 study patients, 60 were males and 40 were females. Characteristics are compared in Table 1. Admission due community-acquired pneumonia was the commonest followed by acute febrile illness. Mean length of ICU stay was 13.6 (standard deviation, SD = 3.75) and mean length of days of mechanical ventilation was 7.93 (SD = 3.89). Mean APACHE II and SOFA scores among ICU survivors at the time of admission was 18.88 (SD = 4.34) and 7.73 (SD = 1.54), respectively.
To test the mean change in different SF-36 variables at baseline, 1 month, and 6 months, RMA was used. It was done at different points of time; and it was found that PCS and MCS scores at pre-ICU were 55.12 and 55.09, respectively (Table 2). Result showed that mean difference was significant at least between one pair for each of the study variables. Multiple pairwise comparisons indicated that the mean difference was significant in all the pairs of SF-36 score, except mental health and vitality. The PCS and MCS scores at 1 month post-discharge deteriorated to 39.59 and 35.49, respectively (p value < 0.05) but at 6 months post-discharge the physical and mental health dimensions showed improvement from baseline.
Correlation of different factors (age, severity of illness, ICU stay, and mechanical ventilation) with QoL index at 1 month and 6 months post-discharge showed that age, APACHE II, and SOFA scores had significant effect on all the components of physical and mental health scores in ICU survivors (Figs 1 to 3). To study the effect of age on QoL, ICU survivors were distributed into two groups. In all, 66 patients were in <50 years’ age-group and 34 patients were in ≥50 years’ age-group. Significant difference was observed in all eight components 1-month post-discharge between the two age-groups (p ≤ 0.05). Patients with age ≥50 years had lower PCS and MCS scores than those <50 years of age (Fig. 1).
Higher severity of illness (APACHE 2 ≥18, SOFA ≥6) significantly affected the QoL post-discharge. A total of 49 patients had APACHE II score ≤18 while 51 had %3E;18. Significant difference was observed in both physical and mental parameters of QoL at 1 month and at 6 months post-ICU discharge (Fig. 2). Similarly 29 patients had SOFA score ≤6 and 71 patients had score >6. Trends in SOFA score were also similar (Fig. 3).
| Characteristics | n (100) |
|---|---|
| Age (years), mean ± SD | 40.62 ± 11.99 |
| Sex (n) | |
| Male | 60 |
| Female | 40 |
| Diagnosis | |
| Community acquired pneumonia | 24 |
| Acute febrile illness | 20 |
| Sepsis with septic shock | 16 |
| Acute liver failure | 12 |
| Subacute pancreatitis | 12 |
| Myocarditis | 8 |
| Exacerbation of COPD | 8 |
| Comorbidity | |
| Diabetes mellitus (DM) | 10 |
| DM with HTN | 7 |
| Hypertension (HTN) | 3 |
| Others | 1 |
| ICU stay, mean ± SD | 13.64 ± 3.75 |
| APACHE, mean ± SD | 18.88 ± 4.34 |
| SOFA, mean ± SD | 7.73 ± 1.54 |
| Days of mechanical ventilation [DONV], mean ± SD | 7.93 ± 3.89 |
Data are presented as mean ± standard deviation where applicable
| Change in mean values during follow-up | |||||||
|---|---|---|---|---|---|---|---|
| Variables, mean ± SD | Pre-ICU admission | At discharge | After 6 months | RMA | Multiple comparisons (p value) | ||
| 1 | 2 | 3 | 1 vs 2 | 1 vs 3 | 2 vs 3 | ||
| PF_NBS | 56.54 ± 1.81 | 38.90 ± 5.26 | 49.39 ± 3.66 | <0.001 | <0.001 | <0.001 | <0.001 |
| RP_NBS | 55.41 ± 2.87 | 31.47 ± 5.36 | 40.99 ± 6.24 | <0.001 | <0.001 | <0.001 | <0.001 |
| BP_NBS | 60.97 ± 3.58 | 51.73 ± 7.86 | 56.81 ± 8.47 | <0.001 | <0.001 | <0.001 | <0.001 |
| GH_NBS | 46.89 ± 8.74 | 30.84 ± 5.55 | 33.88 ± 7.24 | <0.001 | <0.001 | <0.001 | 0.003 |
| VT_NBS | 57.29 ± 4.85 | 42.02 ± 4.78 | 40.42 ± 7.56 | <0.001 | <0.001 | <0.001 | 0.047 |
| SF_NBS | 54.23 ± 4.82 | 26.96 ± 6.48 | 36.78 ± 7.62 | <0.001 | <0.001 | <0.001 | <0.001 |
| RE_NBS | 55.26 ± 1.83 | 32.28 ± 6.45 | 41.13 ± 6.69 | <0.001 | <0.001 | <0.001 | <0.001 |
| MH_NBS | 56.47 ± 3.83 | 42.34 ± 7.60 | 42.34 ± 7.24 | <0.001 | <0.001 | <0.001 | 0.99 |
| PCS | 55.12 ± 3.51 | 39.59 ± 4.65 | 47.93 ± 4.60 | <0.001 | <0.001 | <0.001 | <0.001 |
| MCS | 55.09 ± 3.49 | 35.49 ± 6.36 | 37.46 ± 7.42 | <0.001 | <0.001 | <0.001 | 0.02 |
Data are presented as mean ± standard deviation. The p value <0.05 significant RMA, repeated-measures analysis of variance; PF, physical functioning; RP, role physical-bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role emotional; MH, mental health; NBS, norm-based score; PCS, physical component summary score; MCS, mental component summary score
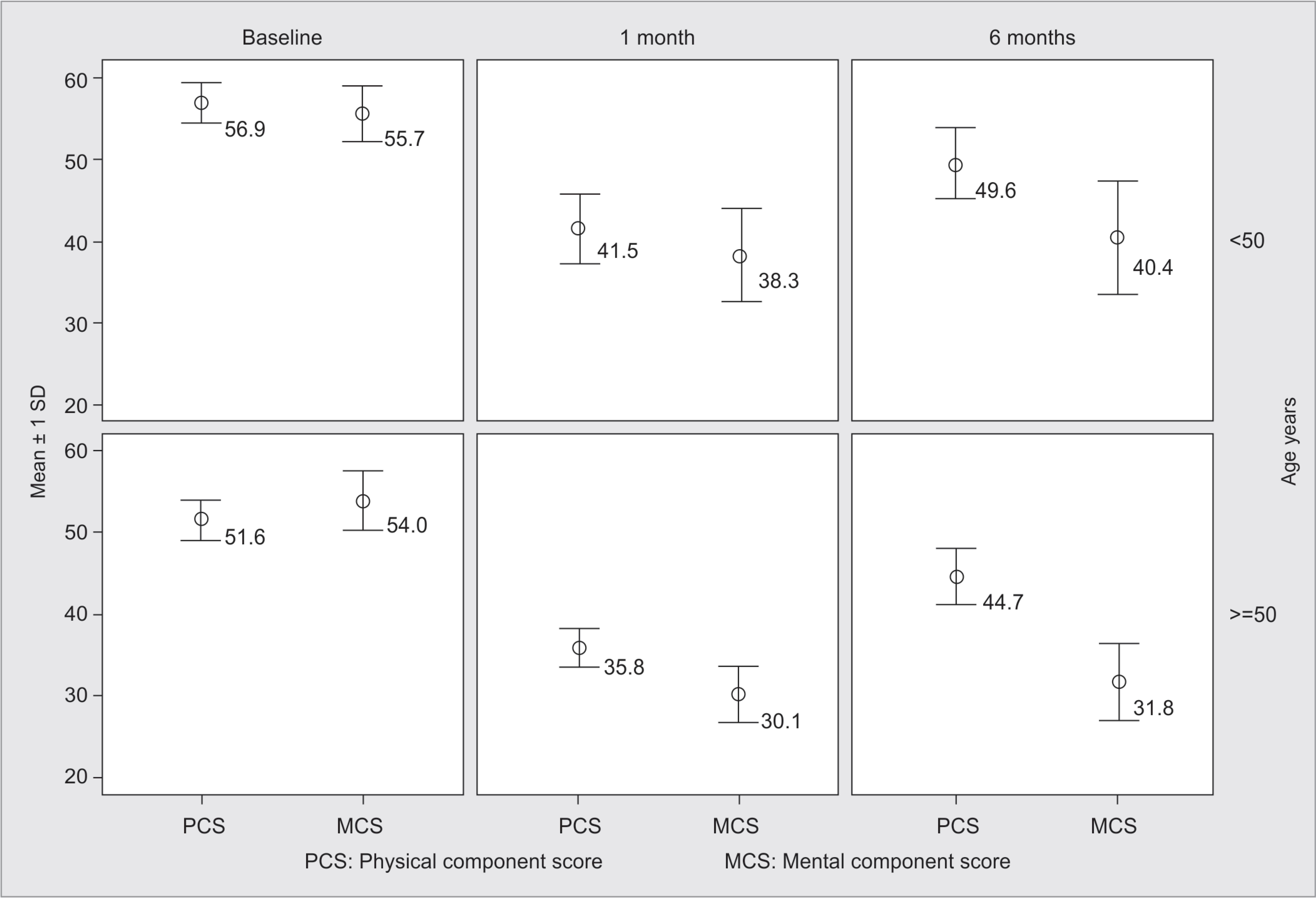
Fig 1:: Error bar graph showing change in PCS and MCS scores (mean ± SD) over the time between baseline to 1 and 6 months with age
Gender of the patient, length of ICU stay, and number of days of mechanical ventilation during ICU stay had no significant correlation at 1 month, while after 6 months’ follow-up significant effect was only seen in PF. Univariate analysis showed no mean difference in statistical significance for MCS and PCS between age-groups, ICU stay, days of mechanical ventilation, and APACHE and SOFA scores; resultant multivariate analysis was not used.

Fig 2:: Error bar graph showing change in PCS and MCS scores (mean ± SD) over the time between baseline to 1 and 6 months with SOFA
The QoL (PCS and MCS scores) showed marked deterioration in the percentage of population lying at or above the general population norm at 1 month and 6 months post-discharge when compared with pre-ICU state in all four components, respectively (Fig. 4).
DISCUSSION
The survivors of critical illness are at risk of permanent or temporary physical and functional deficits affecting QoL. The ideal outcome for a patient is to return to their previous QoL before their stay in ICU or to that expected for a person of the similar age and medical condition.12 However, recovery from critical illness is usually prolonged and varied and depends upon both physical and psychological experiences during critical illness which negatively impacts the QoL.13 Establishing the actual extent or quantification of these problems is difficult and challenging.14 Previous studies have attributed the following factors to affect QoL post-discharge such as age, gender, severity of illness (APACHE II and SOFA scores), duration of mechanical ventilation, and length of stay.6,8,15
On assessing HRQoL using SF-36 questionnaire of all ICU survivors and comparing all eight components of SF36 at pre-ICU status, 1 month after discharge, and 6 months after discharge, significant deterioration was found in both physical and mental parameters (Table 2). Trends in the parameters of QoL showed significant improvement in physical and mental parameters from 1 month post-discharge to 6 months post-discharge in most components, except vitality and mental health. However, these parameters were still lower at 6 months post-discharge as compared to the pre-ICU status (Table 2). These results were similar to many previous studies of ICU patients to assess the QoL post-discharge.1,11,16 Ridley et al. concluded in their study that intensive care impairs the QoL in almost all parameters of QoL.17 Similarly, Steenbergen et al. found that ICU survivors had a significantly lower HRQoL compared to a control group, and around half of the patients did not return directly to their previous level of health after discharge from ICU situation.13 The study by Orwelius et al. observed that most significant decrease in the QoL was observed in physical domains of the QoL, and hardly any difference was observed in the rest of the parameters of the QoL before ICU admission and 6 months after critical illness.2 According to most of the studies, the deterioration in patients’ QoL after ICU discharge occurred mostly because of physical derangements due to critical illness during ICU stay. After a period of critical illness, patients often find themselves unable to accomplish even the simple daily activities. In our study we found more deterioration in mental health dimension than in physical health dimension 1-month post-discharge in ICU survivors. Both PCS and MCS at pre-ICU were 55.12 and 55.09, respectively, and PCS and MCS at 1 month post-discharge were 39.59 and 35.49, respectively. At 6 months’ post-discharge, more significant improvement was seen in physical health than in mental health dimension (PCS at 6 months = 47.93 and MCS = 37.46).

Fig 3:: Error bar graph showing change in PCS and MCS scores (mean ± SD) over the time between baseline to 1 and 6 months with APACHE II
On analyzing the correlation of different factors such as age, gender, length of ICU stay, severity of illness (APACHE II and SOFA scores), and days of mechanical ventilation on different components of QoL index, it was observed that age (Fig. 1), APACHE II score (Fig. 2), and SOFA score (Fig. 3) at time of admission had significant effect on all components of SF-36 scores. Literature supports that age is associated with poorer physical function and general health perceptions and vitality.11,16,18 Studies using other scores such as PF (SF-36), usual activities (EQ-5D), and physical or total QOL (SIP) have found significantly lower values in older vs younger ICU patients.15 We also obtained similar results. The distribution of ICU survivors in the two age-groups demonstrated that 66 patients were <50 years and 34 were ≥50 years. Patients with age ≥50 years have lower PCS (35.84 ± 2.44) and MCS (30.12 ± 3.37) scores (Fig. 1). In a study in UK, it was found that poor physical scores for HRQoL in those under 65 years compared with the UK norm population proved that ICU admission is associated with a significant burden of ill-health.19
Association between severity of illness (APACHE II and SOFA scores) and lower PF or general health perceptions has been consistent with the previous studies.18,20,21 In previous studies, higher APACHE II score, longer length of stay in the ICU,22 and prolonged mechanical ventilation23 have been found to significantly affect the HRQoL after the ICU stay.23,24 Among the patients taken in our study, significant difference was observed in all eight components of mental and physical health dimensions based on APACHE II score at 1 month post-ICU discharge. Patients with higher APACHE II scores (≥18) at the time of admission have lower (worst) scores than those with lower APACHE II scores. At 6 months also significant difference was found between two groups of patients in all parameters (Fig. 2). Similarly trends were seen in 71 patients who had a SOFA score ≥6. Significant difference was found in all parameters of HRQoL at both 1 month and 6 months post-ICU discharge (Fig. 3). Cuthbertson et al. found that premorbid physical components of QoL did appear to be poorer in those with high severity of illness and those with significant comorbidity. No correlation with reduced QoL and organ failure based on SOFA score was established in this study.11 They found deterioration in post-discharge QoL when compared to that before critical illness.
Intensive care-dependent factors (length of stay in the ICU, length of MV, and degree of organ dysfunction during the stay in the ICU) have influenced post-ICU QoL.1 Griffiths et al. demonstrated a marked reduction in all components of QoL both at 6 and 12 months. Around 50% of patients reported problems with mobility, compared with their premorbid state. In their study, many patients required help with self-care before their acute illness; but its percentage increased at 6 months and 1 year post-ICU discharge. Significantly more patients were experiencing moderate or extreme pain and also anxiety and depression.25 In our study, the PCS scale showed marked deterioration in the percentage of population lying at or above the general population norm at 1 month compared with pre-ICU state in all four components (Fig. 4). At 6 months, though the percentage population lying at or above the general population norm increased from that of 1 month post-discharge, but it remained lower than that of the pre-ICU state (Fig. 4). Cheung et al. in their single-center cohort study found that survivors of ARDS, 2 years post-discharge had lower than normal functionality and poor HRQoL. Apart from emotional role and mental health, all other domains remained below that of the normal population.26 We also analyzed MCS score and it showedmarked deterioration in percentage of population lying at or above the general population norm at 1 month compared with the pre-ICU state in all four components. Analysis showed marked deterioration in the percentage of population lying at or above general population norm at 1 month compared with the pre-ICU state in all four components. At 6 months, though the percentage of population lying at or above the general population norm increased from that of 1 month post-discharge, it remained lower than that of pre-ICU state (Fig. 4). In contrast to our study findings, Cuthbertson et al. in their study compared the physical scores for QoL with the general population norm before ICU admission and found it to be low. These components decreased at 3 months and slowly increased back to baseline at 1 year but this was not the case with mental component scores.11 However, their follow-up period was long and could have been associated with better outcomes.

Fig 4:: Sample compared with normal population with respect of MCS ad PCS at baseline, 1 month, 6-month (*uses normative data from quality metric 2009 general population sample)
Psychological outcomes after intensive care include PTSD, “an anxiety disorder that often follows exposure to an extreme stressor that causes injury, threatens life or physical integrity”.27 Possible factors that might have contributed to the outcome could be chronic premorbid condition, psychological history, or sociodemographic factors, such as low socioeconomic position.27 Psychological problems can be classified as anxiety, depression, post-traumatic stress, and cognitive dysfunction, and these can negatively influence perceptions of subsequent health status and HRQoL.28,29 Studies addressing these issues must be carried out in the future to assess the burden on physiological ill health in Indian population.
Limitations in our study were that baseline QoL was obtained retrospectively from survivors or from their proxies. Reliability of relative assessment could be criticized due to different and personalized perceptions. Recall was based on the patient’s memory, which could be biased. Sample size of our study was small. This modest sample size study could not be restricted to a single disease population as the patients with different primary diagnosis and comorbidities were included in the study. The duration of study could be extended to assess further changes in QoL with time. Normative data about HRQoL of Indian population are unavailable; hence data of European general population were taken.
CONCLUSION
There is a strong correlation between age and severity of illness based on APAHCHE II and SOFA scores with QoL at 6 months after discharge from the ICU. When compared to the general population, the QoL of survivors of critical illness was lower at 1 month and 6 months. This study significantly contributes to the data about QoL of Indian population and later can be used to formulate normative data about the QoL of Indian population.
Annexure
Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India Working Proforma
Project–“Impact of Critical Illness on Quality of Life after Intensive Care Unit Discharge”
Date:_______
Name:_______
Age/Sex:_______
Date of hospital admission:_______
Date of discharge:_______
Diagnosis at admission:_______
Preexisting comorbidities with duration:_______
APACHE II ICU at Admission:_______
SOFA ICU at admission:_______
Total days of hospitalization:_______
Total days of mechanical ventilation:_______
Status at discharge:_______
CNS-GCS:_______
Oxygen therapy:_______
Urine output:_______
Oral intake:_______
C.R. No.:_______
Total days of ICU stay:_______
Address:_______
Phone:_______ E-mail ID:_______
Acknowledgments
The authors thank the survivors of ICU and their families who have contributed so much time and effort to this study and have persevered with long-term follow-up.
REFERENCES
1. Badia X, Diaz-Prieto A, Gorriz MT, Herdman M, Torrado H, Farrero E, et al. Using the Euro-Qol-5D to measure changes in quality of life 12 months after discharge from an intensive care unit. Intensive Care Med 2001;27(12):1901–1907. DOI: 10.1007/s00134-001-1137-x.
2. Orwelius L, Teixeira-Pinto A, Lobo C. The role of memories on health-related quality of life after intensive care unit care: an unforgettable controversy? Patient Relat Outcome Meas 2016;7:63–71. DOI: 10.2147/PROM.S89555.
3. Steenbergen S, Rijkenberg S, Adonis T. Long-term treated intensive care patients outcomes: the one-year mortality rate, quality of life, health care use and long-term complications as reported by general practitioners. BMC Anesthesiol 2015;15(1):142. DOI: 10.1186/s12871-015-0121-x.
4. Jackson J, Ely EW, Morey M, Anderson V, Denne L, Clune J, et al. Cognitive and physical rehabilitation of intensive care unit survivors: results of the return randomized controlled pilot investigation. Crit Care Med 2012;40(4):1088–1097. DOI: 10.1097/CCM.0b013e3182373115.
5. Janice. R. Life after critical illness: an overview. J Clin Nurs 2013;23:623–663.
6. Desai Sanjay V, Law TJ, Needham DM. Long term complications of critical care. Crit Care Med 2011;39(2):371–379. DOI: 10.1097/CCM.0b013e3181fd66e5.
7. Sullivan M. Quality of life assessment in medicine: concepts, definitions, purposes and basic tools. Nord J Psychiatry 1992;46(2):79–83. DOI: 10.3109/08039489209103305.
8. Guyuatt G. The philosophy of health-related quality of life translation. Qual Life Res 1993;2(6):461–465. DOI: 10.1007/BF00422220.
9. Kapfhammer HP, Rothenhausler HB, Krauseneck T, Stoll C, Schelling G. Posttraumatic stress disorder and health-related quality of life in long-term survivors of acute respiratory distress syndrome. Am J Psychiatry 2004;161(1):45–52. DOI: 10.1176/appi.ajp.161.1.45.
10. Ware J, Snow K, Kosinski M, Gandek B, SF-36 health survey: Manual and interpretation guide Boston, The health institute; 1993.
11. Cuthbertson BH, Roughton S, Jenkinson D, Maclennan G, Vale L. Quality of life in the five years after intensive care: a cohort study. Crit Care 2010;14(1):R6. DOI: 10.1186/cc8848.
12. Chelluri L, Im KA, Belle SH, Schulz R, Rotondi AJ, Donahoe MP, et al. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med 2004;32(1):619. DOI: 10.1097/01.CCM.0000098029.65347.F9.
13. Tian ZM, Miranda DR. Quality of life after intensive care with the sickness impact profile. Intensive Care Med 1995;21(5):422–428. DOI: 10.1007/BF01707411.
14. Myhren H, Ekeberg O, Toien K, Karlsson S, Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Crit Care 2010;14(1):125. DOI: 10.1186/cc8870.
15. Hofhuis JG, Spronk PE, van Stel HF, Schrijvers GJ, Rommes JH, Bakker J. The impact of critical illness on perceived health-related quality of life during ICU treatment, hospital stay, and after hospital discharge: a long-term follow-up study. Chest 2008;133(2):377–385. DOI: 10.1378/chest.07-1217.
16. Eddleston J, White P, Guthrie E. Survival, morbidity, and quality of life after discharge from intensive care. Crit Care Med 2000;28(7):2293–2299. DOI: 10.1097/00003246-200007000-00018unders Company; 1995.
17. Ridley S. Non‐mortality outcome measures. In ed. S Ridley ed., Outcomes in critical care, Oxford: Butterworth‐Heinemann; 2002. p. 32.
18. Pettila V, Kaarlola A, Makelainen A. Health-related quality of life of multiple organ dysfunction patients one year after intensive care. Intensive Care Med 2000;26(10):1473–1479. DOI: 10.1007/s001340000629.
19. Cuthbertson BH, Scott J, Strachan M. Quality of life before and after intensive care. Anaesthesia 2005;60(4):332–339. DOI: 10.1111/j.1365-2044.2004.04109.x.
20. Wehler M, Geise A, Hadzionerovic D, Aljukic E, Reulbach U, Hahn EG, et al. Health-related quality of life of patients with multiple organ dysfunction: individual changes and comparison with normative population. Crit Care Med 2003;31(4):1094–1101. DOI: 10.1097/01.CCM.0000059642.97686.8B.
21. Vedio A, Chinn S, Warburton F, Griffiths M, Leach R, Treacher D. Assessment of survival and quality of life after discharge from a teaching hospital general intensive care unit. Clin Intensive Care 2000;11(1):39–46. DOI: 10.3109/tcic.11.1.39.46.
22. Sluys K, Häggmark T, Iselius L. Outcome and quality of life 5 years after major trauma. J Trauma 2005;59(1):223–232. DOI: 10.1097/01.ta.0000173832.01547.cb.
23. Averill PM, Beck GJ. Post-traumatic stress disorder in older adults: a conceptual review. J Anxiety Disord 2000;14(2):133–156. DOI: 10.1016/s0887-6185(99)00045-6.
24. Ely WE, Shintani A, Truman B, Speroff T, Gordon SM, Harrell F, et al. Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. J Am Med Associat 2004;29(14):1753–1762. DOI: 10.1001/jama.291.14.1753.
25. Griffiths J, Hatch RA, Bishop J. An exploration of social and economic outcome and associated health-related quality of life after critical illness in general intensive care unit survivors: a 12-month follow-up study. Crit Care 2013;17(3):R100. DOI: 10.1186/cc12745.
26. Cheung AM, Tansey CM, Tomlinson G. Two-year outcomes, health care use, and costs of survivors of acute respiratory distress syndrome. Am J Respir Crit Care Med 2006;174(5):538–544. DOI: 10.1164/rccm.200505-693OC.
27. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed., Washington DC: American Psychiatric Association; 1994.
28. Hutchings A, Raine R, Brady A, Wildman M, Rowan K. Socioeconomic status and outcome from intensive care in England and Wales: a prospective cohort study. Med Care 2004;42(10):943–951. DOI: 10.1097/00005650-200410000-00002.
29. Davydow D, Gifford J, Desai S, Bienvenue O, Needham D. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med 2009;35(5):796–809. DOI: 10.1007/s00134-009-1396-5.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.