REVIEW ARTICLE | https://doi.org/10.5005/jp-journals-10071-23684 |
Awake Proning: Current Evidence and Practical Considerations
1Department of Critical Care, Deep Hospital, Ludhiana, India
2Department of Critical Care Medicine, Bhatia Hospital, Mumbai, Maharashtra, India
Corresponding Author: Gunjan Chanchalani, Department of Critical Care Medicine, Bhatia Hospital, Mumbai, Maharashtra, India, Phone: +91 9757169559, e-mail: gunj80@gmail.com
How to cite this article Sodhi K, Chanchalani G. Awake Proning: Current Evidence and Practical Considerations. Indian J Crit Care Med 2020;24(12):1236–1241.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Prone positioning has been shown to improve oxygenation for decades. However, proning in awake, non-intubated patients gained acceptance in the last few months since the onset of coronavirus (COVID-19) pandemic. To overcome the shortage of ventilators, to decrease the overwhelming burden on intensive care beds in the pandemic era, and also as invasive ventilation was associated with poor outcomes, proning of awake, spontaneously breathing patients gathered momentum. Being an intervention with minimal risk and requiring minimum assistance, it is now a globally accepted therapy to improve oxygenation in acute hypoxemic respiratory failure in COVID-19 patients. We thus reviewed the literature of awake proning in non-intubated patients and described a safe protocol to practice the same.
Keywords: Acute respiratory distress syndrome, Awake proning, Awake self-proning, COVID pneumonia, COVID-19..
INTRODUCTION
The coronavirus disease (COVID-19) presents with a multitude of clinical manifestations, with very high morbidity and mortality. The concern for increased mortality among patients needing invasive ventilation and the shortage of intensive care unit (ICU) beds and ventilators in the pandemic, led to the use of awake proning as a potential strategy to delay intubation or avoid ICU admissions.
Recent reports in COVID-19 acute respiratory distress syndrome (C-ARDS) have shown that awake, self-proning improves oxygenation in this group of patients. We hence reviewed the literature of awake proning and suggested a protocol based on the available evidence.
Proning has been widely studied mainly in intubated ARDS patients and has shown improvement in oxygenation and reduced mortality in patients on invasive ventilation, in large randomized trials.1 However, with increasing clinical experience of treating COVID-19 patients, self-proning of conscious, awake, non-intubated patients with C-ARDS has shown profound improvement in oxygenation, leading to delay and even avoiding intubation and invasive ventilation altogether.
PHYSIOLOGICAL BENEFITS WITH PRONING
Patients in a supine position have compromised pulmonary function, due to
- Atelectasis of the dorsal alveoli.
- Over-inflation of ventral alveoli due to increased respiratory drive.
- Ventilation-perfusion mismatch.
Proning in ARDS has shown to improve survival, possibly explained by the reduction in ventilator-induced lung injury (VILI), as first theorized by Albert2 in 1997. Using personalized computer-simulated models of lung ventilation in 31 obese patients (11 healthy, 20 asthmatics), Foy et al.3 demonstrated the benefits of proning by reducing ventilator heterogeneity and improving ventilation. These effects were more pronounced in patients with a body mass index (BMI) >30 kg/m2.
Figure 1 shows the schematic representation of the lung in the supine (Fig 1A) and prone (Fig 1B) position. Prone positioning (PP) of conscious patients with C-ARDS has shown to improve oxygenation.
The proposed mechanisms explaining the improved oxygenation after awake proning are:
- More uniform distribution of tidal volume and end-expiratory lung volume, thus reducing the cyclical opening and closing of alveoli (reduced atelectasis).4
- Recruitment of areas in the posterior part of the lung, thus improving compliance, and decreasing the shunt.
- Decreased lung deformation (increased homogeneity) and lungs are less compressed in prone, thereby increased ventilation.
- Dorsal lung regions have a higher density of blood vessels (which is independent of gravity). Proning improves the ventilation in these nondependent lung fields, thereby improving the ventilation:perfusion (V:Q) matching.5
- Increased perfusion toward the anterior alveoli; improving the V:Q ratio.
- The chest wall compliance reduces, as the anterior part of the chest is now facing the bed surface, reducing the regional lung stress and potentially decreasing the possibility of patient self-inflicted lung injury (p-SILI). Contraction of muscular diaphragm exerts a more uniform distribution of stress.
- Better secretion drainage.
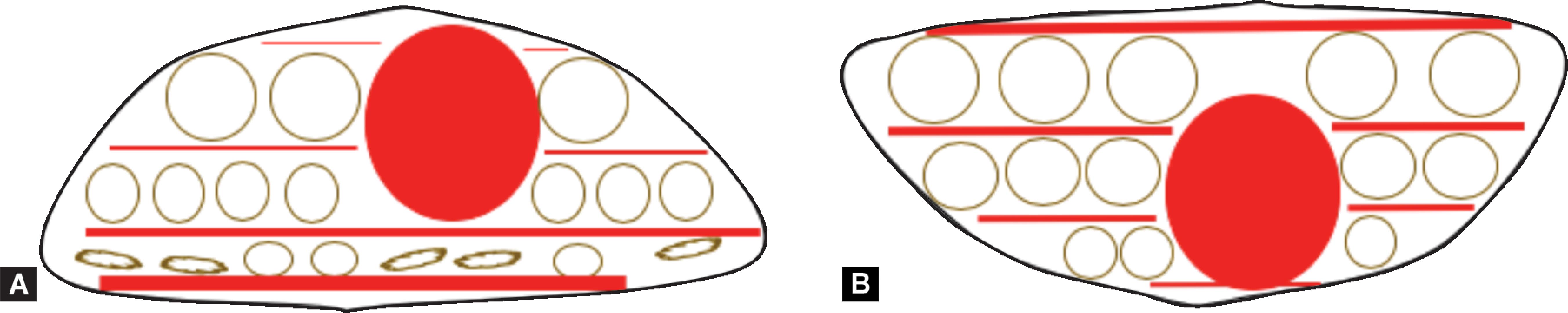
Figs 1A and B: Schematic representation of the lung in the supine (A) and prone (B) position. (The red circle is the heart, the red lines are the blood vessels, and the circles are the alveoli.) (A) In supine position, there is more collapse of the alveoli posteriorly, with overdistention of the ventral alveoli. Perfusion is more in the posterior regions, causing V:Q mismatch. (B) In a prone position, there is the recruitment of the dorsal alveoli and improved V:Q ratio
THE EVIDENCE
There is enormous literature suggesting that PP can increase PaO2/FiO2 (PF) ratio and reduce mortality in moderate-to-severe ARDS and PP has been proposed as a standard treatment during mechanical ventilation in ARDS. But very few studies have reported the use of PP in spontaneously breathing patients.
Pre-COVID Evidence
The first report of the use of awake proning in improving oxygenation dates back to 1977, where proning in one non-intubated patient improved oxygenation and avoided invasive ventilation.6 Further reports of PP in spontaneously breathing patients were reported by Valter et al.7 in 2003. They showed a beneficial effect of PP with spontaneous breathing in four awake patients with hypoxemic respiratory failure in whom mechanical ventilation was indicated. There was rapid improvement in PaO2 and intubation was avoided in all the patients. All four patients had good tolerance to proning.
Feltracco et al.8 showed spontaneous clearance of bronchial secretions, significant attenuation of graft infiltrates and consolidations, reduction in the number of bronchoscopies required, decrease in spontaneous respiratory rate and work of breathing, and a significant improvement in gas exchange with the use of noninvasive ventilation (NIV) with high-frequency percussive ventilation (HFPV) in the prone position of three patients with post-lung transplantation respiratory complications. All three patients were comfortable or only mildly uncomfortable with HFPV by facial mask in the prone position.
Feasibility and efficacy of awake proning were further evaluated in a 6-year retrospective study of 15 spontaneously breathing non-intubated patients with hypoxemic acute respiratory failure in a single Italian ICU.9 Patients underwent 43 PP procedures. Twelve patients were discharged and three died. No complications occurred and no alteration was observed in hemodynamics or respiratory rate. Two procedures were interrupted due to intolerance. In the subset of PP procedure with the same positive end-expiratory pressure (PEEP) and FiO2 (n = 18), significant improvement in oxygenation was observed (p %3C; 0.001) with PaO2/FiO2 increasing from pre-proning 124 ± 50 to 187 ± 72 mm Hg during proning and PaO2/FiO2 remaining elevated post-proning to 140 ± 61 mm Hg. There was no effect on pH or PaCO2 with a change in positioning. In subset of patients on NIV with proning (n = 10), improved oxygenation was observed during proning (PaO2/FiO2 = 214 ± 71 mm Hg) as compared to pre- (157 ± 44 mm Hg) and post-proning (160 ± 69 mm Hg) (p < 0.001).
A prospective multicentric observational cohort study by Ding et al.10 was performed across two teaching hospitals where non-intubated moderate-to-severe ARDS patients with baseline SpO2 ≤ 95%, were placed in PP along with NIV or with high-flow nasal cannula (HFNC), for 2 hours twice daily. The efficacy of four support methods — HFNC, HFNC + PP, NIV, and NIV + PP, in improving oxygenation were evaluated by blood gas analysis. Twenty patients (10 with moderate ARDS and 10 with severe ARDS) were enrolled. Patients were divided into success (11 patients) and failure (9 patients) groups based on whether an intubation was avoided or those who needed intubation, respectively. It was seen that all seven patients with a PaO2/FiO2 < 100 mm Hg on NIV required intubation. PaO2/FiO2 in HFNC + PP was non-significantly higher in the success group than in the failure group (125 ± 41 vs 119 ± 19 mm Hg, p = 0.043). An upward trend in oxygenation (PaO2/FiO2) was seen in all four support strategies: HFNC < HFNC + PP ≤ NIV < NIV + PP. The investigators concluded that patients with severe ARDS were not appropriate candidates for HFNC/NIV + PP.
In another report of three cases of acute respiratory failure secondary to unspecified pneumonia, with PP started due to lack of response to a combination of HFNC and BiPAP over the first 48 hours of admission, a continued improvement was seen over the following 7 days to repeated episodes of PP with HFNC and all patients were discharged from hospital.11
Evidence during the COVID-19 Pandemic
During the COVID-19 pandemic, the use of awake, self-proning increased in cases of hypoxemic respiratory failure. Initially, anecdotal evidence on the benefit of awake proning in COVID-19 was reported, but later more and more evidence has been published on the same.
One of the first reported uses of awake proning in COVID-19 patients was from three Chinese hospitals.12 Of 79 patients with COVID-19, 10 had severe ARDS (PaO2/FiO2, i.e., PF < 300) and had undergone PP along with HFNC. The targets were PP of %3E;16 hours and SpO2 > 90%. After proning, the PF improved significantly in all patients in 3 days and none of them needed intubation. Median PaCO2 increased slightly after proning but was statistically significant (32.3 vs 29.7 mm Hg; p < 0.001). Thereby early awake proning with HFNC was proposed as a therapy to avoid invasive mechanical ventilation in severe ARDS in COVID patients and also reduce medical resource requirement.
In another experience from Jiangsu province13 in China, lower mortality was shown in COVID-19 with early recognition and intervention which included awake PP. Awake proning resulted in significant improvement in oxygenation and pulmonary heterogeneity.
Another pilot observational cohort study was carried out in a single emergency department (ED) in New York City14 which included 50 patients having COVID-19 with hypoxia (SpO2 < 90%). Median SpO2 at triage was 80% (IQR 69–85) which increased with supplemental oxygen to 84% (IQR 75–90) and after 5 minutes of proning to 94% (IQR 90–95). Comparison of the pre- to post-median SpO2 was significant (p = 0.001). Thirteen patients (24%) had no improvement in oxygenation and required endotracheal intubation within 24 hours of arrival to the ED.
Elharrar et al.15 presented a prospective before and after, single-center, French hospital study of 24 patients with acute hypoxemic respiratory failure and infiltrates on computerized tomography (CT) chest. Of 88 patients with COVID-19, 24 non-intubated spontaneously breathing patients requiring supplemental oxygen underwent awake proning. Sixty-three percent were able to tolerate PP for >3 hours. In patients who sustained PP for ≥3 hours, PaO2 increased from 73.6 mm Hg pre-proning to 94.9 mm Hg post-proning. However, oxygenation increased during PP in only 25% and was not sustained in half of those after resupination.
In a 1-day cross-sectional study in 15 awake patients with mild to moderate ARDS, Sartini and colleagues16 applied sessions of PP along with continuous positive airway pressure (CPAP) in medical wards. All patients had a significant reduction in respiratory rate during and after proning (p < 0.001), significant improvement in SpO2 and PF during proning (p < 0.001). Eighty percent of patients had improvement in oxygenation after pronation, 13% had no improvement while 6.7% had worsened parameters after pronation.
In a Singapore study17 of 10 COVID-19 pneumonia patients requiring supplemental oxygen inwards underwent 1-hour session each of prone position, five sessions a day, each 3 hours apart. Hemodynamics and oxygenation at 0, 30, and 60 minutes from the start of each session were monitored. Patients underwent protocol for a median of 21 hours. Nine patients were successfully weaned off oxygen in a median of 8 days. Three patients were shifted to ICU due to increasing oxygen requirement, of which one was subsequently intubated and died from severe ARDS. The other two continued with the same prone protocol and recovered. The study clearly demonstrated the positive effects of the self-proning maneuver on patients’ oxygenation and outcomes.
Similar results were seen in Italy, where Coppo and colleagues18 enrolled 56 confirmed COVID-19-related pneumonia receiving supplemental oxygen or noninvasive CPAP, who were proned for a minimum duration of 3 hours. In 47 patients (83.9%), PP was feasible (i.e., maintained for at least 3 hours). Oxygenation substantially improved from supine to PP (PaO2/FiO2 ratio 180.5 ± 76.6 mm Hg in supine position vs 285.5 ± 112.9 mm Hg in a prone position; p < 0.0001). Improved oxygenation was maintained in 23 patients (50.0%) after resupination but this was not significant compared with before PP (PaO2/FiO2 ratio 192.9 ± 100.9 mm Hg 1 hour after resupination; p = 0.29). Twenty-eight percent of patients were eventually intubated. Five patients died due to underlying disease. The study again showed that PP was feasible in awake patients with COVID-19-related pneumonia and effective in improving oxygenation, with effects maintained after supination in half of the patients.
In a study in Columbia University,19 all consecutive patients admitted to the step-down unit between April 6 and April 14, 2020 (n = 88) with laboratory-confirmed COVID-19 with severe hypoxemic respiratory failure [respiratory rate (RR) ≥ 30 breaths/minute or SpO2 ≤ 93%] receiving supplemental oxygen 6 L/minute via nasal cannula and 15 L/minute via non-rebreather face mask (NRBM) were included. Among 29 eligible patients, 25 had at least one awake session of the prone position lasting longer than 1 hour; four refused the prone position and were intubated immediately. SpO2 improved from 1 to 34% (median [SE], 7% [1.2%]; 95% CI, 4.6% to 9.4%). One hour after initiation of the prone position, 19 patients had SpO2 of ≥95% and 7 patients (37%) required intubation. Among six patients whose SpO2 remained <95% 1 hour after initiation of the prone position, five (83%) were intubated. Among 12 who required intubation, 3 died subsequently in the ICU.
Few case reports of self-proning in COVID-19 patients having respiratory distress have come up since the inception of the pandemic. All patients had good outcomes with an improvement in their PF ratio that allowed the oxygen requirement to be reduced and invasive ventilation could be avoided.20–22
Ongoing Trials
Optiprone (Prone Positioning During High Flow Oxygen Therapy in Acute Hypoxemic Respiratory Failure: A Pilot Physiological Trial) (NCT03095300) is a pilot feasibility study to assess the safety and efficacy of PP in acute hypoxemic respiratory failure patients, noninvasively treated with HFNC. Estimated enrollment is 15 patients and each enrolled patient will be monitored in the supine position for one hour, placed in the prone position for 2 hours, and replaced in the supine position for a final 1-hour step. The study is expected to be complete in December 2020.
ProCov (Prone Positioning in Spontaneously Breathing Nonintubated COVID-19 Patient: A Pilot Study) (NCT04344106) is an open-label clinical trial which included 25 COVID-19 patients with posterior lung involvement who may benefit from prone position sessions before mechanical ventilation. The study has been completed and the results are awaited.
APPROVE-CARE (Awake Prone Positioning to Reduce invasive VEntilation in COVID-19 induced Acute Respiratory failure) (NCT04347941) is an ongoing multicenter open-label randomized control trial on 200 participants to determine if PP reduces the need for mechanical ventilation. As per the study protocol, PP will be given for at least 16 hours a day with 45 minutes break for meals. The study results are expected in mid-2021.
COVI-PRONE (Awake Prone Position in Hypoxemic Patients With Coronavirus Disease 19: A Randomized Clinical Trial) (NCT04350723) is an ongoing multicenter randomized control trial over 350 participants to determine if early awake PP in COVID-19 patients with hypoxemic respiratory failure; irrespective of the mode of oxygen delivery; reduces the need for invasive mechanical ventilation. The secondary outcomes to be measured are mortality, invasive, and NIV free days, ICU and hospital length of stay, change in oxygenation and complications from proning.
Another ongoing clinical trial is the Study of High-Flow Nasal Cannula with Prone Position for COVID-19 Acute Respiratory Distress Syndrome which is a multicenter randomized controlled trial of early use of PP combined with HFNC COVID-19-induced moderate-to-severe acute respiratory distress syndrome (20032604-IRB01). The study aims to prove that early use of PP combined with HFNC can improve oxygenation and reduce the need for intubation in COVID-19-induced moderate-to-severe ARDS patients.
Thus, multiple trials have shown that awake self-proning in non-intubated patients, helps improve the oxygenation and avoid intubation in many. We propose the following protocol and safety process to be followed while encouraging awake proning in your unit with COVID-19 hypoxemic respiratory failure.
PROTOCOL FOR AWAKE PRONING
All patients with COVID-19 lung involvement should be encouraged to lie prone, as it is a low-cost, low-risk maneuver requiring minimal manpower. It can be safely done in the wards, outside the ICU in mild to moderate severity of the disease. However, frequent monitoring of such patients should be done on the floors, to look for early deterioration and need for shifting to ICU in case of worsening.
The Intensive Care Society23 has recently advocated for a trial of PP in conscious patients with suspected/confirmed COVID-19 requiring FiO2 of ≥28% or requiring basic respiratory support to maintain SpO2 92–96% (or 88–92% in those at risk of hypercapnic respiratory failure), utilizing cycles of 30 minutes to 2 hours, rotating through prone to right-sided to supine to left-sided positioning.
Flowchart 1 shows the process to follow while proning a patient of COVID-19 hypoxemic respiratory failure.
Indications of Awake Proning
- All patients with SpO2 %3C;94% and RR %3E;22/minute should be advised early awake proning.
Though the benefits of awake proning in mild COVID-19 disease have not been studied, the strategy should be encouraged in this group of patients as well.
- Patients on oxygen supplementation via nasal prongs, oxygen mask, NRBM, HFNC, and NIV, can be safely self-proned, as per their tolerance and comfort.

Flowchart 1: Steps to follow when we awake prone a conscious patient
Whom Can We Awake Prone?
- Conscious, cooperative, alert patients who can self-communicate.
- Able to adjust their own position, with minimal assistance.
How to Do Awake Proning?
- Explain the procedure to the patient and its benefits.
- Emphasize to maintain the position for 30 minutes to 2 hours.
- Alternative lateral and semi-prone positions may be tried if the patient is unable to prone completely.
- In anxious patients, low doses of anxiolytics may be considered to improve tolerance. However, a close watch for respiratory depression should be kept.24
Care during Awake Proning
- Continue monitoring of vitals—SpO2, respiratory rate, pulse rate, blood pressure.
- Initial monitoring should be every 15 minute for the first 30 minutes; thereafter every 30–60 minutes till in PP.
- Vigilant monitoring to detect early signs of deterioration.
- A call bell should be available.
- Patients with a protruding abdomen will need a special mattress for the same. The use of multiple pillows/towels to create a hollow in the middle of the patient’s abdomen may be tried.
Contraindications to Awake Proning25
Mild tachycardia, tachypnea, and hypoxemia are not considered as a contraindication to conscious proning. However, awake proning should be avoided in the following group of patients:
- Patients in need of immediate intubation.
- Compromised airway.
- Respiratory exhaustion.
- Uncooperative patients.
- Patients with altered mentation.
- Hemodynamic instability, arrhythmias.
- Patients with an unstable spine, pelvic instability, chest trauma, recent abdominal surgery.
- Pregnancy: second and third trimester.
How Long do We do Awake Proning?
Studies have shown that although a single proning episode improves PaO2, the effect of a single episode of proning is usually ill-sustained. Hence, we advise prolonged and repeated episodes of conscious proning to help consistent improvements. The optimal duration for awake proning has not to be studied, and its lot depends on the patient body habitus, tolerance, and comfort in the prone position.
A single session of a prone position should be maintained for at least 120 minutes for an effective improvement in oxygenation. It is advisable to do frequent proning to an average of 5 to 6 hours per day.
When to Interrupt?
There is no specific recommendation for how long a patient should be self-proned. We suggest that awake, self-proning should be continued till the patient is comfortable, or has recovered and maintaining oxygen saturation >96% on room air, and has no respiratory distress/desaturation on exertion.
In a sick patient, proning should be interrupted if there is evidence of increased work of breathing, use of accessory muscles of respiration, failure of improvement in oxygenation with proning/further desaturation, or hemodynamic instability/arrhythmias.
An improvement in oxygen saturation on awake proning should not be an assurance of the improvement in the disease condition. Vigilance should be kept for signs of respiratory distress or increased work of breathing, which are an indication to interrupt awake proning and the need for invasive ventilation. The decision to intubate and invasively ventilate should be based on clinical assessment of work of breathing and other clinical criteria. Delaying intubation, just due to improvement in oxygenation can lead to catastrophic outcomes.26
CONCLUSION
While robust data are lacking, awake self-proning has been shown to improve oxygenation in COVID-19 patients in multiple observational studies. It may not successfully prevent all intubations but is a zero-cost tool to use with minimal complications. Its effects on mortality are yet to be studied in controlled trials. Though it appears promising, careful, and frequent monitoring of patients requiring high oxygen flows is recommended. Also, whether awake proning will help in non-C-ARDS, is yet an unanswered question, but it may be a potential low-cost therapeutic option in an acute hypoxemic respiratory failure of all causes.
REFERENCES
1. Guérin C, Reignier J, Richard JC, Beuret P, Gacouin A, Boulain T, et al. Prone positioning in severe acute respiratory distress syndrome. N. Engl. J. Med. 2013;368(23):2159–2168. DOI: 10.1056/NEJMoa1214103.
2. Albert RK. The prone position in acute respiratory distress syndrome: where we are, and where do we go from here. Crit. Care Med. 1997;25(9):1453–1454. DOI: 10.1097/00003246-199709000-00006.
3. Foy BH, Brightling CE, Siddiqui S. Proning reduces ventilation heterogeneity in patients with elevated BMI: implications for COVID-19 pneumonia management? ERJ Open Res 2020;6(2):00292–02020. DOI: 10.1183/23120541.00292-2020.
4. Cornejo RA, Díaz JC, Tobar EA, Bruhn AR, Ramos CA, González RA, et al. Effects of prone positioning on lung protection in patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care. Med. 2013;188(4):440–448. DOI: 10.1164/rccm.201207-1279OC.
5. Glenny RW, Lamm WJ, Albert RK, Robertson HT. Gravity is a minor determinant of pulmonary blood flow distribution. J. Appl. Physiol. 1991;71(2):620–629. DOI: 10.1152/jappl.1991.71.2.620.
6. Douglas WW, Rehder K, Beynen FM, Sessler AD, Marsh HM. Improved oxygenation in patients with acute respiratory failure: the prone position. Am. Rev. Respir. Dis. 1977;115(4):559–566. DOI: 10.1164/arrd.1977.115.4.559.
7. Valter C, Christensen AM, Tollund C, Schønemann NK. Response to the prone position in spontaneously breathing patients with hypoxemic respiratory failure. Acta Anaesthesiol. Scand. 2003;47(4):416–418. DOI: 10.1034/j.1399-6576.2003.00088.x.
8. Feltracco P, Serra E, Barbieri S, Milevoj M, Michieletto E, Carollo C, et al. Noninvasive high-frequency percussive ventilation in the prone position after lung transplantation. Transplant. Proc. 2012;44(7):2016–2021. DOI: 10.1016/j.transproceed.2012.05.062.
9. Scaravilli V, Grasselli G, Castagna L, Zanella A, Isgrò S, Lucchini A, et al. Prone Positioning improves oxygenation in spontaneously breathing nonintubated patients with hypoxemic acute respiratory failure: a retrospective study. J. Crit. Care 2015;30(6):1390–1394. DOI: 10.1016/j.jcrc.2015.07.008.
10. Ding L, Wang L, Ma W, He H. Efficacy and safety of early prone positioning combined with HFNC or NIV in moderate to severe ARDS: a multi-center prospective cohort study. Crit. Care. 2020;24(1):28. DOI: 10.1186/s13054-020-2738-5.
11. Bellone A, Basile A. Prone positioning in severe acute hypoxemic respiratory failure in the emergency ward. Emerg Care J 2018;14(1):22–23. DOI: 10.4081/ecj.2018.7524.
12. Xu Q, Wang T, Qin X, Jie Y, Zha L, Lu W, et al. Early awake prone position combined with high-flow nasal oxygen therapy in severe COVID-19: a case series. Crit. Care. 2020;24(1):250. DOI: 10.1186/s13054-020-02991-7.
13. Sun Q, Qiu H, Huang M, Yang Y. Lower mortality of COVID-19 by early recognition and intervention: experience from Jiangsu Province. Ann Intensive Care 2020;10(1):33. DOI: 10.1186/s13613-020-00650-2.
14. Caputo ND, Strayer RJ, Levitan R. Early self-proning in awake, non-intubated patients in the emergency department: a single ED’s experience during the COVID-19 pandemic. Acad. Emerg. Med. 2020;27(5):375–378. DOI: 10.1111/acem.13994.
15. Elharrar X, Trigui Y, Dols A-M, Touchon F, Martinez S, Prud’homme E, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA 2020;323(22):2336–2338. DOI: 10.1001/jama.2020.8255.
16. Sartini C, Tresoldi M, Scarpellini P, Tettamanti A, Carcò F, Landoni G, et al. Respiratory parameters in patients with COVID-19 after using noninvasive ventilation in the prone position outside the intensive care unit. JAMA 2020;323(22):2338–2340. DOI: 10.1001/jama.2020.7861.
17. Ng Z, Tay WC, Ho CHB. Awake prone positioning for non-intubated oxygen dependent COVID-19 pneumonia patients. Eur. Respir. J. 2020(1): in press 10.1183/13993003.01198-2020.
18. Coppo A, Bellani G, Winterton D, Di Pierro M, Soria A, Faverio P, et al. Feasibility and Physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med 2020;8(8). DOI: 10.1016/S2213-2600(20)30268-X.
19. Thompson AE, Ranard BL, Wei Y, Jelic S. Prone Positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Int Med 2020;180(11):1537–1539. DOI: 10.1001/jamainternmed.2020.3030.
20. Slessarev M, Cheng J, Ondrejicka M. Patient self-proning with high-flow nasal cannula improves oxygenation in COVID-19 pneumonia. Can J Anesth 2020(9):19–21. DOI: 10.1007/s12630-020-01661-0.
21. Elkattawy S, Noori M. A case of improved oxygenation in SARS-CoV-2 positive patient on nasal cannula undergoing prone positioning. Respir. Med. Case Rep. 2020;30: 101070. DOI: 10.1016/j.rmcr.2020.101070.
22. Sztajnbok J, Maselli-Schoueri JH, Cunha de Resende Brasil LM, de Sousa LF, Cordeiro CM, Borges LM Sansão, et al. Prone positioning to improve oxygenation and relieve respiratory symptoms in awake, spontaneously breathing non-intubated patients with COVID-19 pneumonia. Respir. Med. Case Rep. 2020;30: 101096. DOI: 10.1016/j.rmcr.2020.101096.
23. Intensive Care Society ICS Guidance for prone positioning of the conscious COVID patient. ICS, 2020. Available at www.ics.ac.uk/ICS/COVID-19/COVID-19_Guidance/ICS/GuidelinesAndStandards/COVID19_Guidance.aspx?hkey=fff229b8-28da-43f6-a0d6-f2d50b5fcf68.
24. Paul V, Patel S, Royse M, Odish M, Malhotra A, Koenig S. Proning in non-intubated (PINI) in times of COVID-19: case series and a review. J. Intensive. Care. Med. 2020;35(8):818–824. DOI: 10.1177/0885066620934801.
25. Prasad M, Visrodia K. Should I prone non-ventilated awake patients with COVID-19? Cleve. Clin. J. Med. 2020. Online ahead of print 10.3949/ccjm.87a.ccc050.
26. Telias I, Katira BH, Brochard L. Is the prone position helpful during spontaneous breathing in patients with COVID-19? JAMA 2020;323(22):2265–2267. DOI: 10.1001/jama.2020.8539.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.