ORIGINAL ARTICLE |
https://doi.org/10.5005/jp-journals-10071-23942 |
COVID-19 Pandemic: Impact on Admission, Diagnosis, and Treatment of Non-COVID-19 Patients Admitted to SARI ICU
1Department of Anaesthesia and Critical Care, JSS Medical College and Hospital, Mysuru, Karnataka, India
2Public Health Evidence South Asia, Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal, Karnataka, India
3,5,6Department of Critical Care Medicine, Kasturba Medical College and Hospital, Manipal Academy of Higher Education, Manipal, Karnataka, India
4Department of Data Science, Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal, Karnataka, India
Corresponding Author: Sunil Ravindranath, Department of Critical Care Medicine, Kasturba Medical College and Hospital, Manipal Academy of Higher Education, Manipal, Karnataka, India, Phone: +91 8095800142, e-mail: sunil.r@manipal.edu
How to cite this article: Arunachala S, Venkatesh BT, Bhatt MT, Puranik A, Rao S, Ravindranath S. COVID-19 Pandemic: Impact on Admission, Diagnosis, and Treatment of Non-COVID-19 Patients Admitted to SARI ICU. Indian J Crit Care Med 2021;25(8):853–859.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Background: Coronavirus disease 2019 (COVID-19) pandemic has caused a huge burden on healthcare services worldwide, severely affecting the management of non-COVID-19 patients as well. The Government of India has updated guidelines for the clinical management of COVID-19 illness, including severe acute respiratory infections (SARI) definition for triaging suspected COVID-19 cases in an isolated intensive care unit (ICU). The aim of this study was to estimate the adherence of clinicians in triaging COVID-19 suspects as per SARI definition to SARI ICU. This study also observed the impact of such triaging on admission, diagnosis, and treatment process of non-COVID-19 patients admitted to SARI ICU.
Patients and methods: This cross-sectional study was conducted in a designated SARI ICU of two tertiary care medical college hospitals involving 78 patients from the month of June to July 2020. Data related to demographics, the severity of illness, advanced life supports, delay in diagnosis, intervention, and treatment of patients in SARI ICU due to suspected COVID-19 status were documented.
Results: Adherence to SARI definition for triaging COVID-19-suspect cases was 19.2%. Despite hindrance in diagnosis (17.9%) and treatment (12.8%), mortality among patients in SARI ICU was limited to 14.10%. Results were insignificant when checked for various factors associated with mortality.
Conclusion: Nonadherence to SARI definition may lead to undue delay in diagnosis, intervention, and treatment of non-COVID-19 cases. This may result in increased morbidity, mortality, and economic burden on patients and the healthcare system.
Keywords: COVID-19, Mortality, Pandemic, Severe acute respiratory infection, Treatment and diagnosis delay.
key message: A rationale and just utilization of healthcare resources are need of the hour in the face of an enormous volume of SARI cases during COVID-19 pandemic. SARI criteria as implemented by the Ministry of Health and Family Welfare (MOHFW), Government of India, are a very important tool in triaging of COVID-19-suspect cases. Adequate measures should be in place in order to mitigate the inadequacies and deficiencies in the treatment of non-COVID-19 cases, which have occurred as a result of COVID-19 pandemic.
INTRODUCTION
The coronavirus disease 2019 (COVID-19) was first detected in Wuhan, China, but is now becoming an increasing public concern due to its rapid spread.1,2 While most people with COVID-19 develop only mild illness, approximately 14% develop severe disease requiring hospitalization and oxygen support, and 5% require admission to an intensive care unit (ICU). In severe cases, COVID-19 can be complicated by acute respiratory distress syndrome, septic shock, and multiorgan failure, including acute kidney injury and cardiac injury. Older age, male gender, and comorbid diseases like diabetes mellitus, hypertension, and ischemic heart disease (IHD) have been reported as risk factors for death.3–5
Various countries have strategized their approach at different healthcare levels to cope with the spread of the pandemic. The first confirmed COVID-19 case in India was detected on January 30, 2020. The Government of India laid down interim guidelines, which are upgraded periodically, for clinicians taking care of hospitalized adult and pediatric patients when COVID-19 infection is suspected. The guidelines have defined triaging of suspected COVID-19 patients as per the severe acute respiratory infection (SARI) definition. Patients are triaged at various entry levels, and suspected cases, as per this definition, are isolated to a dedicated wing of the healthcare setup. However, it was seen that a moderate percentage of suspected cases have turned out to be COVID-19 negative, especially during the initial stage of the pandemic.
Though there are no confirmed numbers on active SARI cases in India, estimated numbers are in millions; adding onto humongous burden on workforce resources, finance, and logistical aspects of hospital infrastructure may thereby compromise the quality of care for both COVID-19 and other patients admitted to SARI ICU. This has imposed huge challenges on the tertiary care sector and the other healthcare sectors in India. There has been no study until date that has investigated the impact of adherence to SARI definition during this COVID-19 pandemic on admission, diagnosis, and treatment of non-COVID-19 patients admitted to SARI ICU. This study aimed at filling the gap for the same.
MATERIALS AND METHODS
An Institutional Ethical Clearance was obtained, and the study was registered in the Clinical Trial Registry of India, before enrolling the participants. We followed the STROBE guidelines for the methodology to carry out and report the findings from this study.
Study Design
The cross-sectional study was conducted in 20-bedded designated SARI ICU of two tertiary care medical college hospitals, South India, in the months of June and July 2020. Each center had designated two local coordinators who ensured that all local necessary ethical and regulatory approvals were obtained before the start of the enrollment of eligible patients. Informed consent was either taken from the patient or patient’s immediate kin if the patient was on a mechanical ventilator or had altered neurological status.
All adult patients aged above 18 years presenting with SARI symptoms (history of fever or measured temperature ≥38°C and cough, onset within the last 10 days) or suspicion of COVID-19 as per physician’s discretion were admitted to SARI ICU, which was a COVID-19-suspect ICU in both study centers. Nasopharyngeal and oropharyngeal/tracheal swabs were taken on the day of arrival to SARI ICU for all the patients. Study centers did not have in-house reverse transcriptase-polymerase chain reaction (RT-PCR) testing facility during the study period, and RT-PCR test results took 36 to 48 hours to arrive. After results, confirmed COVID-positive patients were excluded from the study and shifted to designated COVID ICU. COVID-negative patients were moved to non-COVID-19 multidisciplinary ICU. The study aimed to estimate the implications on morbidity and mortality of the COVID-negative patients due to delay in diagnosis, intervention, and treatment during their stay in SARI ICU.
Data Collection
Data related to the following were collected from the inpatient charts: Patient demographic data along with comorbidities, annual income of the patient, and whether health insurance availed. The patient’s presenting complaints were classified into respiratory and nonrespiratory. Adherence to SARI definition and American Thoracic Society (ATS) criteria for ICU admission for community-acquired pneumonia (CAP) were documented.6 Sequential organ failure assessment (SOFA) score was collected at admission.7 Requirements of various organ supports like mechanical ventilation, vasopressor use, and renal replacement therapy were noted. Patient outcomes, such as discharge from ICU and in-hospital mortality, were also documented. Data about the impediment to treatment defined as any delay, change, or failure in diagnosis in SARI ICU, any cross-consultation delay, any hindrance in allied health services due to suspected COVID-19 status while the patient was in SARI ICU were also collected.
The operational definitions for documenting delay in diagnosis, intervention, cross-consultation, and treatment were as follows.
- Delay in diagnosis—Arrival at a working diagnosis after more than 24 hours of admission to SARI ICU was considered as “delay in diagnosis.”
- Delay in intervention—Interventions needed in study patients were case and time-specific; such as intubation, hemodialysis, source control procedures, and delay in intervention were documented as noticed by attending experienced intensivist.
- Delay in cross-consultation—Cross-consultation to specialty disciplines in the study center was real-time involving both written documentation and telephonic intimation. Any cross-consultation pending to be attended even after 4 hours of written documentation and intimation was considered as “delay in cross-consultation.”
- Delay in treatment—Failure to initiate treatment as per working diagnosis even after more than 24 hours of admission to SARI ICU was considered as “delay in treatment.”
Statistical Analysis
The collected patient’s data were analyzed using software SPSS version 16. Care was taken to minimize the errors in data entry and analysis. Data were summarized using mean and standard deviation for normally distributed variables. Median and interquartile range (IQR) was reported for skewed variables. Frequencies of all the categorical data were calculated and summarized using graphs. Fisher’s exact test was performed to assess the relationship of delay in diagnosis, impediment in treatment, age, gender, organ support, and comorbidities with that of mortality. Independent samples t-test was used to detect whether a significant difference in age exists between those who experienced mortality and those who did not. Since the factor onset of symptom delay was not normally distributed, MannWhitney U-test was used to compare the delay between those who experienced mortality and those who did not.
RESULTS
The overall data of a total of 78 patients were collected (Table 1), out of which 31 (39.7%) were females and 47 (60.3%) were males. The mean age of the participants was 55.15 years. The median annual income of the participants was 144,000 (84,000–210,000) INR or 1958 USD, out of which 37 (47%) utilized government schemes, eight (11%) utilized private schemes, and 33 (42%) participants paid cash for hospitalization. Comorbidities of the patients were as mentioned in Table 1. The mean SOFA score was 5.87 with 15 (19.2%) patients admitted fulfilling the SARI definition and 45 (57.7%) patients admitted fulfilling the ATS criteria.
| Age—mean (SD) in years | 55.15 (17.71) |
| Gender (%) | Male: 47 (60.3) Female: 31 (39.7) |
| Patient’s income—median (IQR) | 144000.00 (84000.00, 210000.00) in rupees/annum |
| Percentage of modes of payment by patients | Cash—42% Government schemes—47% Private schemes—11% |
| SOFA score—mean (SD) | 5.87 (4.15) |
| Patients admitted fulfilling the SARI definition (%) | 15 (19.2) |
| Patients admitted fulfilling the ATS criteria (%) | 45 (57.7) |
| Comorbidities | |
| Diabetes mellitus | 30 (38.41%) |
| Hypertension | 27 (34.61%) |
| Cardiac conditions (IHD, heart failure, atrial, and ventricular septal defects) | 17 (21.79%) |
| Respiratory conditions (chronic obstructive pulmonary disease, bronchial asthma, pulmonary Koch’s, and bronchiectasis) | 14 (17.94%) |
| Neurological and psychiatric conditions | 6 (7.69%) |
| Hypothyroidism and other endocrinological diseases | 9 (11.53%) |
| Renal failure | 14 (17.94%) |
| Postsurgery | 1 (1.28%) |
| Malignancy | 3 (3.84%) |
| Other immunosuppressive diseases | 5 (6.41%) |
The majority of the patients admitted to SARI ICU reported nonrespiratory symptoms. Out of 78 patients who were hospitalized, 74% were admitted with nonrespiratory presentations. Out of which 21.79% had constitutional symptoms; 19.23% had gastrointestinal causes, such as abdominal pain, abdominal distension, vomiting, diarrhea, etc.; cardiac causes, such as shortness of breath, palpitation, and chest pain, were seen in 17.94%; and another 17.94% of patients had neurological symptoms, such as seizures, septic encephalopathy, giddiness, etc. Renal symptoms, such as decreased urine output, uremic encephalopathy, and volume overload, were found in 15.38%. Of patients with respiratory symptoms documented, shortness of breath was observed in 15.38%, cough in 12.82%, and productive sputum in 3.84% of patients (Fig. 1).

Fig. 1: Pie chart showing mode of presentation of patients to SARI ICU
It was observed that the majority of patients were not on advanced life supports (43%). At least 19% were on invasive mechanical ventilation and vasopressors both, 13% were on invasive mechanical ventilation alone, and 1% were on noninvasive mechanical ventilation. Five percent of patients were on vasopressor therapy alone, 9% on renal replacement therapy alone, and only 1% on combined vasopressor support and renal replacement therapy, as depicted in Fig. 2. Delay in diagnosis, cross-consultation, intervention, and treatment are represented in Fig. 3. The majority of patients (66%) admitted to SARI ICU were discharged from the hospital; 19% were discharged against medical advice. The overall mortality of non-COVID-19 patients in SARI ICU during the study period was 14.10%. The results, when checked for gender, respiratory, and nonrespiratory comorbidities, and delay in diagnosis and treatment with that of mortality, were not significant as depicted in Table 2. Details of patients expired, including basic demographics, illness severity scoring, clinical presentation, diagnosis, delay in diagnosis, intervention, and treatment, are described in Table 3.

Fig. 2: Pie chart showing the requirement of organ support requirement for patients in SARI ICU
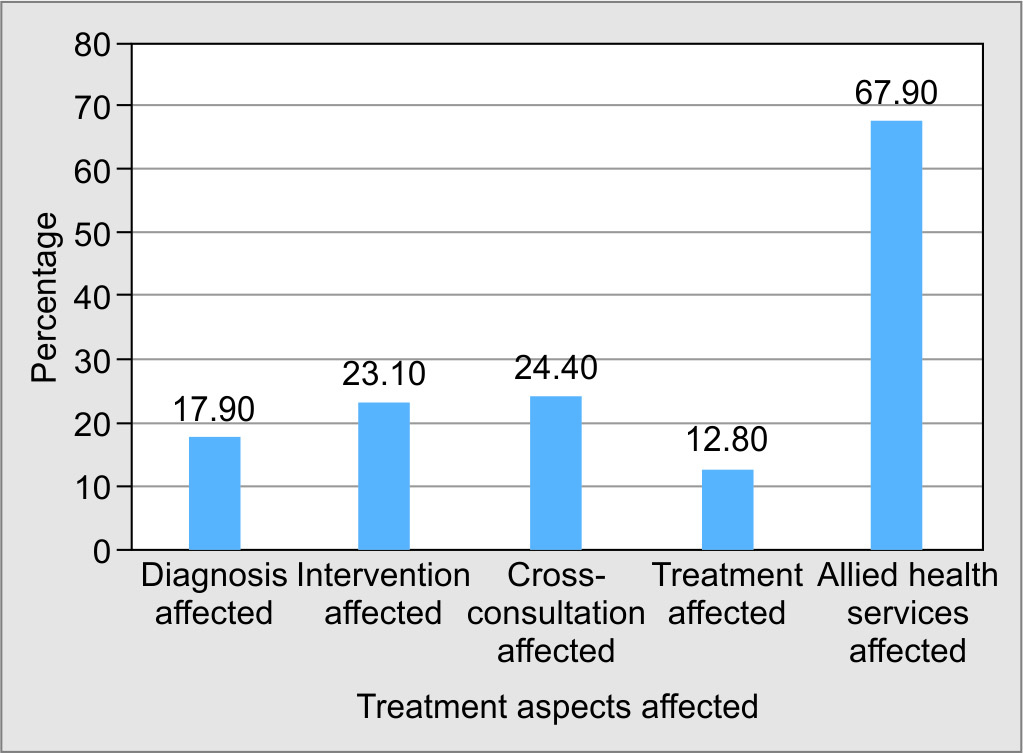
Fig. 3: Impediment in treatment (delay in diagnosis, intervention, cross-consultation, and treatment) of non-COVID-19 patients in SARI ICU
| Mortality | Delay in diagnosis | Delay in treatment | Organ Support | Respiratory comorbidity | Nonrespiratory comorbidity | Gender | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | No | Yes | No | Yes | Female | Male | |
| No (%) | 53 (82.8) | 14 (100.0) | 57 (83.8) | 10 (100.0) | 42 (91.3) | 25 (78.1) | 23 (92.0) | 44 (83.0) | 15 (83.3) | 52 (86.7) | 29 (93.5) | 38 (80.9) |
| Yes (%) | 11 (17.2) | 0 (0.0) | 11 (16.2) | 0 (0.0) | 4 (8.7) | 7 (21.9) | 2 (8.0) | 9 (17.0) | 3 (16.7) | 8 (13.3) | 2 (6.5) | 9 (19.1) |
| No. | Age in years/sex | Comorbidities and final diagnosis | Complaints | Fulfilling SARI criteria | SOFA | Delay | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Diagnosis | Intervention | Cross-consultation | Treatment | Investigation | ||||||
| 1 | 76/F | Nil premorbid | Nonrespiratory | No | 2 | No | No | Cardiology reference | No | No |
| Pulmonary edema secondary to non-ST elevation, myocardial infarction, heart failure with reduced ejection fraction | ||||||||||
| 2 | 58/M | Nil premorbid | Nonrespiratory | No | 8 | No | Yes | No | No | Ultrasonography of abdomen |
| Acute pancreatitis, multiorgan dysfunction syndrome | ||||||||||
| 3 | 53/M | Diabetes, hypertension, old cerebrovascular accident, multinodular goiter | Nonrespiratory | No | 4 | No | No | Neurology reference | No | Magnetic resonance imaging of brain |
| Cardioembolic stroke | ||||||||||
| 4 | 35/M | Nil premorbid | Nonrespiratory | No | 14 | No | No | No | No | Computed tomography of abdomen |
| Pancreatitis Leptospirosis Multiorgan dysfunction syndrome Alcohol dependence syndrome |
||||||||||
| 5 | 36/F | Diabetes, post-tuberculosis bronchiectasis | Nonrespiratory | No | 4 | No | No | Cardiology reference | No | No |
| Congestive cardiac failure post-tuberculosis bronchiectasis | ||||||||||
| 6 | 49/M | Diabetes, hypertension, chronic kidney disease | Nonrespiratory | No | 5 | No | No | No | No | No |
| Pulmonary edema secondary to volume overload, acute coronary syndrome | ||||||||||
| 7 | 64/M | Diabetes, hypertension | Nonrespiratory | No | 15 | No | No | Cardiology reference | No | No |
| Cardiogenic shock | ||||||||||
| 8 | 55/M | Traumatic paraplegia | Respiratory | No | 10 | No | No | No | No | No |
| CAP, septic shock | ||||||||||
| 9 | 63/M | Diabetes, hypertension | Respiratory | Yes | 9 | No | No | No | No | No |
| CAP, septic shock | ||||||||||
| 10 | 54/M | Diabetes, hypertension, chronic kidney disease, psoriasis | Respiratory | No | 19 | No | No | No | No | No |
| CAP | ||||||||||
| 11 | 20/M | Diabetes | Respiratory | Yes | 17 | No | No | Nephrology reference | No | No |
| CAP, diabetic ketoacidosis, multiorgan dysfunction | ||||||||||
DISCUSSION
There were 1, 81,859 confirmed and 89,729 active COVID-19 cases in India at the beginning of the study. Apart from protocols and clinical management guidelines from the Ministry of health and family welfare (MOHFW), the Government of India vouched for social distancing measures such as lockdown that spanned over two and a month period in four different phases (March 24, 2020–June 8, 2020). Despite measures like lockdown, screening, testing, and triaging, India witnessed single-day spikes of more than 1,000 cases in almost every state. With the process of unlock in the near-future evident, the total number of confirmed cases was expected to rise, and it is, therefore, necessary to utilize the limited healthcare resources rationally.
The Government of India has laid down SARI definition for triaging of suspected COVID-19 cases.8
SARI was defined as “an acute respiratory illness with history of fever or measured temperature ≥38°C and cough, onset within the last ~10 days and requiring hospitalization.”
Surveillance case definition for COVID-19 was defined as “severe acute respiratory infection (SARI) in a person, with history of fever and cough requiring admission to hospital, with no other etiology that fully explains the clinical presentation (clinicians should also be alert to the possibility of atypical presentations in patients who are immunocompromised). It also included any of the following:
- A history of travel to Wuhan, Hubei Province, China, in the 14 days prior to symptom onset;
- The disease occurs in a healthcare worker who has been working in an environment where patients with severe acute respiratory infections are being cared for, without regard to the place of residence or history of travel;
- The person develops an unusual or unexpected clinical course, especially sudden deterioration despite appropriate treatment, without regard to the place of residence or history of travel, even if another etiology has been identified that fully explains the clinical presentation.”
Initial phase of the pandemic not only witnessed inadequacies in the management of COVID-19 population but also impacted the diagnosis and treatment of non-COVID-19 patients as well. Guidelines put forth by the MOHFW, Government of India, had advised triaging of COVID-19 suspects as per SARI definition. However, the researchers observed shortcomings in triaging these COVID-19-suspect patients as per SARI definition upon hospitalization, which resulted in unwarranted admission of non-COVID-19 patients in SARI ICU, resulting in undue delay in the management of such cases. Hence, the study was conceptualized to determine the impact of nonadherence to SARI definition triaging COVID-19 suspects in diagnosis and management of non-COVID-19 patients in SARI ICU. Adherence of clinicians to SARI definition while admitting suspected patients to ICU was 19.2%. Reasons for nonadherence to SARI definition in triaging can be multifactorial. Firstly, triaging of COVID-19 suspects to SARI ICU was left to the physician’s discretion. There might have been a cautious approach in triaging these cases as we were still in the early phase of pandemic, and robust knowledge on clinical presentation, including atypical symptoms, was still lacking. Lack of knowledge of SARI definition among clinicians and fear of in-hospital clustering of COVID-positive cases could also have contributed to this.
Shortness of breath was the commonest presenting complaint, of which only 15.38% had a respiratory cause. This indicates to the fact that fear among clinicians could have contributed to the unwarranted admission. Nonetheless, among the admitted SARI cases, nearly 57.7% had fulfilled the ATS criteria for admission to ICU in cases of severe CAP, suggesting that majority did require ICU care but may not SARI ICU. Adherence to SARI definition can be improved by proper training of the physicians and updating them about recent guidelines.
The mean age of our study participants and comorbidities were comparable to that of INDICAPS study and STRIDE study.9,10 Mean SOFA score was also similar to that of ICON study suggesting that the study population was representative of a general ICU population.11 The operational definitions for delay in diagnosis, intervention, cross-consultation, and treatment were based on previous studies.12–14 The impediments in diagnosis, intervention, cross-consultation, treatment, and allied health services care to the patient were restricted to 17.9, 23.1, 12.8, 24.4, and 67.9%, respectively. Nursing care including administering intravenous medications, feeding, bowel, and bladder care was largely unaffected as the nurse-to-patient ratio of 1:1 was implemented for the clinical care. However, there was an undue delay in sending laboratory investigations to microbiology, pathology, and critical care laboratories, procuring medicines from in-hospital pharmacies, and intrahospital transfer of patients for investigations due to limited housekeeping staffs, which could not be documented. The hindrance for allied health services was mainly physical rehabilitation and dietary services. Despite diagnosis and treatment being affected in 17.9 and 12.8% of cases, respectively, the patient’s discharge from hospital was 66%.
Overall mortality during the study period was 14.10%. One percent of the patient population was considered for palliative care during the hospital stay. Compared to medical ICUs involved in USCIITG-CIOS study, mortality was lower in our study.15 Percentage of patients requiring mechanical ventilation, vasopressors, and renal replacement therapy was higher compared to KIND study, yet mortality was marginally lower in our study.16 Thus, despite the uncertain scenario involved with an ongoing pandemic, the study population was treated with appropriate care. The mean SOFA score of the expired population was 9.72. There was some delay in cross-consultation from super-specialty disciplines, as depicted in Table 3. Reasons for low rates of mortality of non-COVID-19 patients in SARI ICU despite nonadherence to SARI definition triaging them can be many. SARI ICU’s in study centers had qualified intensivists providing clinical expertise round the clock assuring there is no delay in diagnosis and intervention despite inadequacies in cross-consultations (24.4%) and investigations. However, the same cannot be generalized to other healthcare settings that do not have round the clock intensivist cover where nonadherence to triaging as per SARI definition in such settings might result in higher mortality rates. Our study had limitations in having a small sample size, and we need similar studies in the future to confirm the findings.
It is interesting to note that nearly 47% of the study population had availed government-run health insurance schemes, and 11% had used private health insurance compared to only 16% insured patients in INDICAPS study.9 This could be due to the extensive availability and implementation of government health schemes in study centers. The average cost of SARI ICU stay per day in two study centers was INR 25,000 per day. This is higher than the average cost of a regular ICU stay that is around INR 15,000 per day. There were considerable unquantified monetary implications observed by investigators during the study; for example, the finance involved in revamping existing hospital infrastructure into dedicated COVID-19 ICU, education of healthcare workers regarding infection control practices, additional use of sanitizers, personal protective equipment, N95 masks, and complete shutdown of elective surgical procedures. In the earlier phase of the pandemic, these two study centers did not have in-house RT-PCR testing available. RT-PCR test results would take at least 24 to 48 hours to arrive, leading to increased length of stay of non-COVID-19 patients in SARI ICU. This could have increased the financial burden on non-COVID-19 patients and also depriving highly resourceful intensive care beds to actual COVID-19-suspect patients. Even though we intended to capture this economic data initially, it could not be done due to the lack of manpower and funding.
The study had its own limitations. The mean SOFA score of patients under study in SARI was 5.87. SOFA scores were calculated on the first day of ICU admission only and might not be reflective of sequential worsening of organ functions later in the ICU stay. We defined non-COVID-19 patients as those whose first RT-PCR was negative. Since RT-PCR has approximately 63 and 32% sensitivity for nasal and throat swabs, respectively, this definition may have been flawed, and suspected patients might mandate repeat RT-PCR if the pretest probability of patients having COVID-19 is high.17,18 It was an observational cross-sectional study involving two tertiary care medical college hospitals. The findings cannot be generalized unless it is done on a larger scale involving multiple centers. The decreased sample size in this study was due to the restrictions that were laid due to the pandemic situation that decreased the access for data collection.
Despite these limitations, our study had major strengths. This is one of the first studies to our knowledge to evaluate outcome variables like failure or change in diagnosis, delay in intervention, treatment, and investigations affecting clinical management and mortality of non-COVID-19 patients in this pandemic scenario. The study also projects challenges and management of non-COVID-19 patients at tertiary care sectors. Further studies on a larger scale are mandated to evaluate the guidelines in triaging of COVID-19-suspect cases for better utilization of healthcare resources in the treatment of patients during these trying times and to project the needs to overcome the barriers to enhance the treatment for non-COVID-19 patients during the pandemic.
CONCLUSION
Adherence to SARI definition while triaging COVID-19-suspect cases to ICUs was low. There were hindrances in the diagnosis and treatment of non-COVID-19 patients due to admission to SARI ICU as COVID-19 suspects. However, treatment outcomes of these patients were comparable to the critically ill population with similar disease severity scoring suggesting that quality of care may not have been compromised despite the pandemic. Poor adherence to SARI definition while triaging might have led to economic implications on patients and healthcare systems, but further studies are required before generalizing the findings.
ACKNOWLEDGMENTS
We would like to express our gratitude to Dr. Purva Makhija, Dr. Devika Anil, Dr. Harinaveen, and Dr. Rituparna Bordoloi, postgraduates from the Department of Anaesthesiology, Kasturba Medical College, Manipal, and postgraduates from the Department of Anaesthesiology, JSS Medical College and Hospital, Mysuru, for their immense contribution in data collection for the research. The authors would also like to thank Dr. Sriram Sampath, Dr. Gurudatt CL, Dr. Ravi MD, Dr. Chetak, and Dr. Mahesh PA, for their valuable inputs during the preparation of this manuscript.
Clinical Trial Registry India number—REF/2020/05/033786.
The manuscript has been read and approved by all authors, criteria of authorship for each author have been met, and each author believes that the manuscript is a reflection of sheer hard work, honesty, and devotion toward the research.
ORCID
Sumalatha Arunachala https://orcid.org/0000-0001-5858-8298
Bhumika T Venkatesh https://orcid.org/0000-0002-3338-6478
Margiben Tusharbhai Bhatt https://orcid.org/0000-0002-8966-1096
Amitha Puranik https://orcid.org/0000-0003-2047-9453
Shwethapriya Rao https://orcid.org/0000-0002-5635-5332
Sunil Ravindranath https://orcid.org/0000-0003-4022-1492
REFERENCES
1. World Health Organization [homepage on the Internet]. Geneva: WHO characterizes COVID-19 as a pandemic [cited 2020 March 11]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-asthey-happen.
2. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382(13):1199–1207. DOI: 10.1056/NEJMoa2001316.
3. Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020;8(5):475–481. DOI: 10.1016/S2213-2600(20)30079-5 [Erratum in: Lancet Respir Med 2020;8(4):e26]. PMID: 32105632; PMCID: PMC7102538.
4. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. China medical treatment expert group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382(18):1708–1720. DOI: 10.1056/NEJMoa2002032. PMID: 32109013; PMCID: PMC7092819.
5. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult in patients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395(10229):1054–1062. DOI: 10.1016/S0140-6736(20)30566-3 [Erratum in: Lancet 2020;395(10229):1038]. PMID: 32171076; PMCID: PMC7270627.
6. Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America; American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007;44(Suppl. 2):S27–S72. DOI: 10.1086/511159. PMID: 17278083; PMCID: PMC7107997.
7. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med 1996;22(7):707–710. DOI: 10.1007/BF01709751. PMID: 8844239.
8. Guidelines on clinical management of severe acute respiratory illness (SARI) in suspect/confirmed novel coronavirus (nCoV) cases. Available from: https://main.mohfw.gov.in/sites/default/files/Guidelines%20on%20Clinical%20management%20of%20severe%20acute%20respiratory%20illness.pdf.
9. Divatia JV, Amin PR, Ramakrishnan N, Kapadia FN, Todi S, Sahu S, et al; INDICAPS Study Investigators. Intensive Care in India: The Indian intensive care case mix and practice patterns study. Indian J Crit Care Med 2016;20(4):216–225. DOI: 10.4103/0972-5229.180042. PMID: 27186054; PMCID: PMC4859158.
10. Mk MV, Krishna B, Sampath S. Secular trends in an Indian intensive care unit-database derived epidemiology: the stride study. Indian J Crit Care Med 2019;23(6):251–257. DOI: 10.5005/jp-journals-10071-23175. PMID: 31435142; PMCID: PMC6698356.
11. Vincent JL, Marshall JC, Namendys-Silva SA, François B, Martin-Loeches I, Lipman J, et al; ICON investigators. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med 2014;2(5):380–386. DOI: 10.1016/S2213-2600(14)70061-X. PMID: 24740011.
12. Álvarez-Lerma F, Marín-Corral J, Vila C, Masclans JR, de Molina FJ, Loeches IM, et al. Delay in diagnosis of influenza A (H1N1) pdm09 virus infection in critically ill patients and impact on clinical outcome. Crit Care 2016;20(1):337. DOI: 10.1186/s13054-016-1512-1.
13. Soares DM, Pessanha JF, Sharma A, Brocca A, Ronco C. Delayed nephrology consultation and high mortality on acute kidney injury: a meta-analysis. Blood Purif 2017;43(1–3):57–67. DOI: 10.1159/000452316.
14. Martínez ML, Ferrer R, Torrents E, Guillamat-Prats R, Gomà G, Suárez D, et al. Impact of source control in patients with severe sepsis and septic shock. Crit Care Med 2017;45(1):11–19. DOI: 10.1097/CCM.0000000000002011.
15. Checkley W, Martin GS, Brown SM, Chang SY, Dabbagh O, Fremont RD, et al; United States critical illness and injury trials group critical illness outcomes study investigators. Structure, process, and annual ICU mortality across 69 centers: United States critical illness and injury trials group critical illness outcomes study. Crit Care Med 2014;42(2):344–356. DOI: 10.1097/CCM.0b013e3182a275d7. PMID: 24145833; PMCID: PMC4035482.
16. Park J, Jeon K, Chung CR, Yang JH, Cho YH, Cho J, et al. A nationwide analysis of intensive care unit admissions, 2009–2014 – The Korean ICU National Data (KIND) study. J Crit Care 2018;44:24–30. DOI: 10.1016/j.jcrc.2017.09.017. PMID: 29028553.
17. Arevalo-Rodriguez I, Buitrago-Garcia D, Simancas-Racines D, Zambrano-Achig P, Del Campo R, Ciapponi A, et al. False-negative results of initial RT-PCR assays for COVID-19: a systematic review. PLoS One 2020;15(12):e0242958. DOI: 10.1371/journal.pone.0242958.
18. Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020;323(18):1843–1844. DOI: 10.1001/jama.2020.3786. PMID: 32159775; PMCID: PMC7066521.
________________________
© The Author(s). 2021 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.