CASE REPORT | https://doi.org/10.5005/jp-journals-10071-24082 |
Unilateral Pulmonary Contusion after Cardiopulmonary Resuscitation Complicated by Delayed Obstructive Atelectasis: A Case Report and Review of the Literature
1,2Division of Pulmonary and Critical Care Medicine, Department of Medicine, Faculty of Medicine, Thammasat University, Pathumthani, Thailand
Corresponding Author: Pattarin Pirompanich, Division of Pulmonary and Critical Care Medicine, Department of Medicine, Faculty of Medicine, Thammasat University, Pathumthani, Thailand, Phone: +66-2-9269794, e-mail: pirompanichp@gmail.com
How to cite this article: Klumusuk P, Pirompanich P. Unilateral Pulmonary Contusion after Cardiopulmonary Resuscitation Complicated by Delayed Obstructive Atelectasis: A Case Report and Review of the Literature. Indian J Crit Care Med 2022;26(1):133–135.
Source of support: Nil
Conflict of interest: None
ABSTRACT
We present a previously healthy 57-year-old man who had a sudden cardiac arrest intraoperatively and developed unilateral pulmonary contusion shortly after cardiopulmonary resuscitation. He was gradually improved by supportive management. But, several days later he had worsening of respiratory symptoms and obstructive atelectasis was proven by bronchoscope finding of thick mucus plugging left main bronchus. These are rarely recognized but important post-resuscitation complications. Early detection is crucial to improve outcome.
Keywords: Bronchoscopy, Cardiopulmonary resuscitation, Obstructive atelectasis, Unilateral pulmonary contusion.
INTRODUCTION
Pulmonary contusion is a direct or indirect lung parenchyma damage caused by chest trauma,1 which can be a complication of chest compression during cardiopulmonary resuscitation (CPR).2 Alveolar-capillary membrane is torn by kinetic energy transferring to the lung tissue in injured patients. Consolidation and alveolar collapse occur as a result of blood and proteinaceous fluid flooding alveoli and loss of surfactant. In addition, increased airway mucous production in response to inflammation creates mucous plugging, air resorption, and collapse of injured lung segments.3
The incidence of unilateral pulmonary contusion after CPR is about 10.8% on the left lung and 2.5% on the right lung when detected by autopsy.2 Obstructive atelectasis can be a complication of pulmonary contusion. But the incidence of atelectasis after CPR has not been documented and may cause significant ventilation-perfusion mismatching and lead to a life-threatening condition. We report a case of unilateral pulmonary contusion after CPR which caused obstructive atelectasis several days later.
CASE DESCRIPTION
A 57-year-old man, a glazier, presented to our emergency department after left forearm laceration injury. He had no known underlying disease and was transferred directly to the operating room (OR) for vascular and tendon repair. After repairing his first tendon, he developed pulseless ventricular tachycardia (VT). CPR was started immediately by mechanical chest compression (MeCC) devices. Venoarterial extracorporeal membrane oxygenation (VA-ECMO) was commenced after 39 minutes of CPR and return of spontaneous circulation (ROSC) was achieved. Coronary angiography was immediately performed, which revealed 70% stenosis of left circumflex artery. Percutaneous coronary intervention with drug eluting stent was done successfully. He was still on VA-ECMO and transferred to cardiac care unit (CCU). He was sedated by fentanyl and midazolam and ventilated by pressure assist/control mode of ventilation.
Chest radiograph shortly after ROSC showed increased homogeneous opacity of the entire left hemithorax consistent with left pulmonary contusion (Fig. 1A). Conservative management including mechanical ventilation support, adequate pain control, and regular endotracheal suction were the main treatments of his pulmonary condition, consistent with the standard procedure.4 Chest radiograph showed gradual improvement over the next 3 days (Fig. 1B).
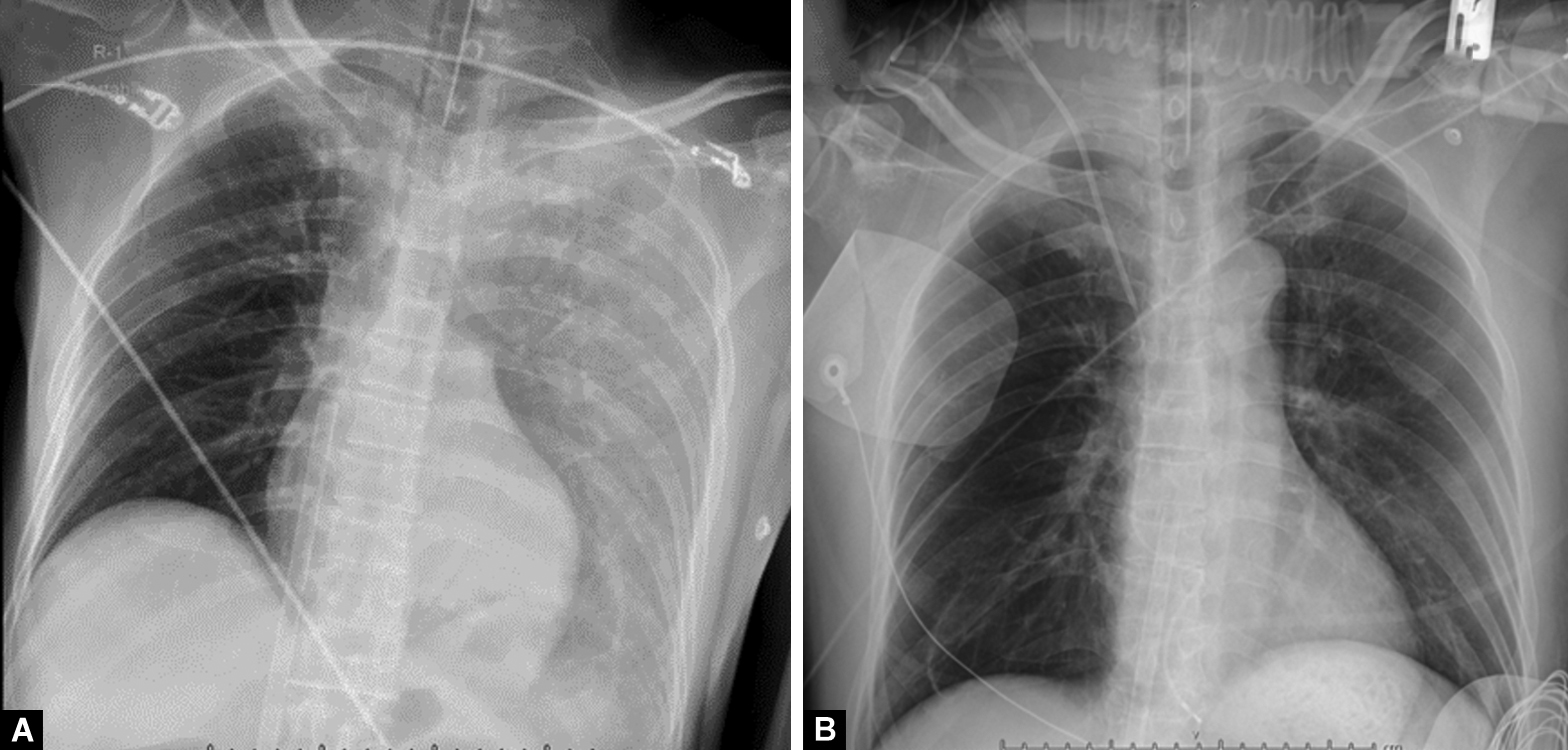
Figs 1A and B: Chest X-ray showing: (A) Increased homogeneous opacity at entire left lung; (B) Improvement of left pulmonary contusion 3 days after supportive treatment
He gradually improved until the fourth day after ROSC, when sudden worsening of dyspnea, agitation, and desaturation occurred. Patient-ventilator asynchrony was inevitable and muscle relaxant was given. Pulmonary auscultation revealed diminished breath sound on left side. Chest radiographs showed complete atelectasis at upper left lung and partial collapse of lower left lung (Fig. 2). Bronchoscopy, performed on the next day, demonstrated total obstruction of the left main bronchus by thick hyper-viscosity mucous secretions (Fig. 3A). After therapeutic bronchoscopy, left side bronchi were all patent (Fig. 3B). His clinical condition improved significantly and ECMO was then decannulated one day after bronchoscopy. Chest radiograph showed full expansion of the left lung after copious mucous was removed. He weaned from ventilator and successfully extubated shortly thereafter.
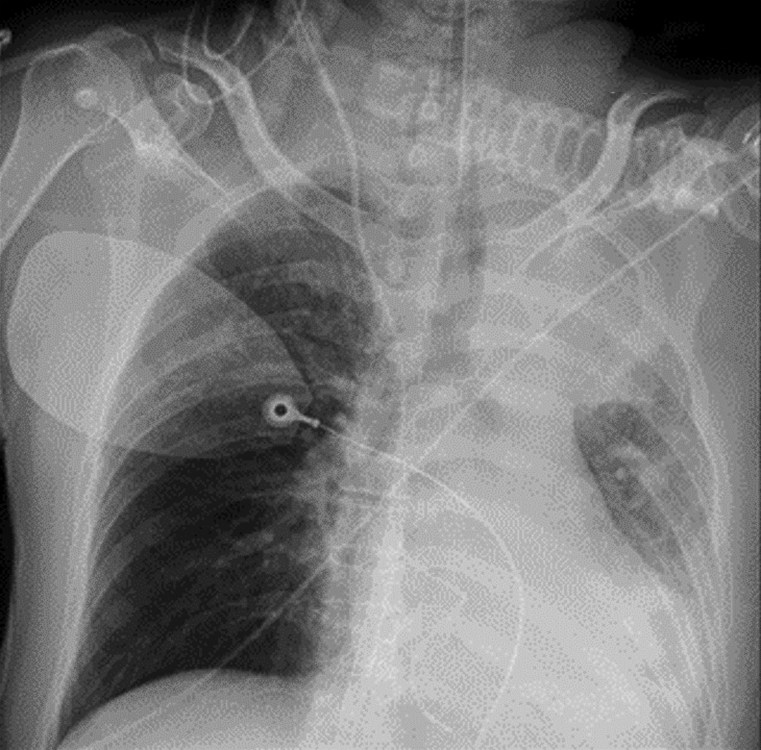
Fig. 2: Chest-X-ray showing homogenous opacity at left upper lobe and left retrocardiac area with left lung volume loss

Figs 3A and B: Bronchoscopic finding of right and left main bronchus. (A) Thick hyperviscosity mucus obstructing left main bronchus; (B) Patient main bronchial lumen after therapeutic bronchoscopy for suction secretion
We obtained written informed consent from the patient. IRB approval was waived because this is a retrospective study.
DISCUSSION
Pulmonary contusion related to CPR is a significant problem in survivors, but there are few studies on this subject. Hellevuo et al.5 found that only one in 134 cases has lung contusion; however, the study does not explain the method of chest compression (traditional hand technique or using a MeCC device).
Pulmonary contusion results in bleeding and fluid leakage into the alveoli and the interstitial space of the lung, causing the lung to become rigid and lose its normal elasticity. Fluid accumulation in alveoli interferes with gas exchange causing ventilation-perfusion mismatching and concomitant loss of surfactant creating consolidation, alveolar collapse, and decrease in compliance. Surfactant activity deficit is most severe 24 hours after contusion.6 The different blood components that enter to the alveoli cause the release of multiple inflammatory mediators. This inflammatory response leads to rising mucous production, plugging part of the lung and resulting in its collapse,6 as seen in our patient. Also, the pain associated with chest wall injury can restrict ventilation and promote atelectasis.
Now, the MeCC device is more frequently used in many clinical settings, especially during the COVID-19 pandemic. There are few medical reports about pulmonary contusion after CPR, especially using the MeCC device. Atelectasis after pulmonary contusion by mucous plugging can increase ventilation-perfusion mismatching and lead to respiratory deterioration. The possibility of atelectasis should be considered when acute desaturation or change of PaO2 correlated with acute dyspnea. Regular daily follow-up chest radiograph is important for several days after CPR. Early detection and management may improve ventilation and reduce subsequent complication.
CONCLUSION
Pulmonary contusion after chest compression is a potential serious complication that is possibly under-reported. Its complication of atelectasis from thick mucus and from surfactant loss might lead to prolonged mechanical ventilation and poor outcome. Early detection of these post-CPR complications is crucial to improve post-cardiac arrest care outcome.
ORCID
Pongpat Klumusuk https://orcid.org/0000-0001-8282-8001
Pattarin Pirompanich https://orcid.org/0000-0003-0181-5394
REFERENCES
1. Rendeki S, Molnar TF. Pulmonary contusion. J Thorac Dis 2019;11(Suppl. 2):S141–S151. DOI: 10.21037/jtd.2018.11.53.
2. Kaldırım U, Toygar M, Karbeyaz K, Arzıman I, Tuncer SK, Eyi YE, et al. Complications of cardiopulmonary resuscitation in non-traumatic cases and factors affecting complications. Egypt J Forensic Sci 2016;6(3):270–274. DOI: 10.1016/j.ejfs.2015.07.005.
3. Sattler S, Maier RV. Pulmonary contusion. In: Karmy-Jones R, Nathens A, Stern EJ, editors. Thoracic trauma and critical care. Boston, MA: Springer US; 2002. p. 235–245. DOI: 10.1007/978-1-4615-1127-4.
4. Lai CC, Wang CY, Lin HI, Wang JY. Pulmonary contusion associated with chest compressions. Resuscitation 2010;81(1):133. DOI: 10.1016/j.resuscitation.2009.10.001.
5. Hellevuo H, Sainio M, Nevalainen R, Huhtala H, Olkkola KT, Tenhunen J, et al. Deeper chest compression–more complications for cardiac arrest patients? Resuscitation 2013;84(6):760–765. DOI: 10.1016/j.resuscitation.2013.02.015.
6. Ganie F, Lone H, Lone GN, Wani ML, Singh S, Dar A, et al. Lung contusion: a clinico-pathological entity with unpredictable clinical course. Bull Emerg Trauma 2013;1(1):7–16. PMID: 27162815; PMCID: PMC4771236.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.