CASE REPORT |
https://doi.org/10.5005/jp-journals-10071-24187 |
Extracorporeal Membrane Oxygenation Support in Refractory Multi-organ Failure by 3,4-Methylenedioxymethamphetamine Intoxication (“Ecstasy”)
1–4Department of Intensive Care Unit, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina
Corresponding Author: Victoria Ruiz, Department of Intensive Care Unit, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina, Phone: +5491141963371, e-mail: victoriaruizprieto@gmail.com
How to cite this article: Ruiz V, Rosciani F, Bisso IC, Heras ML. Extracorporeal Membrane Oxygenation Support in Refractory Multi-organ Failure by 3,4-Methylenedioxymethamphetamine Intoxication (“Ecstasy”). Indian J Crit Care Med 2022;26(4):523–525.
Source of support: Nil
Conflict of interest: None
ABSTRACT
The substance known as 3,4-methylenedioxymethamphetamine (MDMA) that is commonly named ecstasy is a designer drug used for recreation. The intoxication for MDMA could generate hyperthermia, hepatotoxicity, acute renal failure, cardiovascular toxicity, hyponatremia, serotonin syndrome, coma, and, eventually could lead to, death. There is no antidote available, that is why the treatment is symptomatic and of advanced vital support until the resolution of the case. A case is presented of an adult with multi-organ failure secondary to intoxication for MDMA in whom it was decided to initiate support of oxygenation with extracorporeal membrane oxygenation as a bridge to recovery, with good results.
Keywords: Extracorporeal membrane oxygenation treatment, Intensive care, N-methyl-3, 4-methylenedioxyamphetamine.
INTRODUCTION
The substance known as 3,4-methylenedioxymethamphetamine (MDMA) that is commonly named ecstasy is a designer drug that acts directly inhibiting the reuptake of serotonin and belongs to the family of amphetamines.1 Its original use and diffusion were related to electronic parties and rave culture, but nowadays, its consumption was extended outside of that scope.2
The MDMA is absorbed in the intestinal tract and reaches the maximum concentration in plasma approximately 2 hours after oral consumption.3 The substance is degraded metabolically in the liver, mainly through CYP2D6 enzyme, with early enzyme saturation; therefore, small increments of doses could lead to a risk of large increases in toxicity.4 Common doses are between 50 and 200 mg, but if it is ingested in capsules or tablets that are manufactured with no regulation, the quantity of active principle and the quality of the excipients are unknown.1 Even more, the clearance of 95% of the drug is accomplished after 40 hours of use which explains the persistence of secondary effects even 2 days after use.5 There is no antidote available that is why the treatment is symptomatic and of vital support. Measures of aggressive cooling are required with strict monitoring of corporal temperature and adequate reanimation.6
There are scarce reports in the literature that detail extracorporeal membrane oxygenation (ECMO) as a strategy in acute poisoning. A report from the American Society of Toxicology observed 26,271 cases, and stated only 10 patients with ECMO support, even though those presented survival of 80%.7 On the other hand, there are reports of poisoning with substances such as organophosphates,8 aluminum phosphate,9 chloroquine,10 and amlodipine toxicity11 that were successfully treated with extracorporeal devices. There is one report published by Thakkar et al.12 of venovenous ECMO support in a patient intoxicated with MDMA, where the device was used in the context of acute respiratory distress, with concomitant hyponatremia and associated cerebral edema. In all these cases, the results of the use of extracorporeal devices were satisfactory, proving the effectiveness of the treatment as support with a noticeable increase in survival.
We report a case of an adult patient who presented refractory multi-organ failure secondary to MDMA poisoning requiring extracorporeal life support with good response.
CASE DESCRIPTION
A male of 31-years-old with previous problematic drug use entered the emergency department presenting alteration of mental state with psychomotor excitement, neuromuscular rigidity, and hypothermia. Companions referred to him as having taken three tables of ecstasy during the previous 12 hours.
During physical examination, he presented sinus tachycardia (heart rate of 146 heartbeats/minute), central and peripheral cyanosis, oliguria, arterial hypotension (median arterial tension of 41 mm Hg), and fever (39.9°C).
Lab evidenced acute renal failure (creatinine 3.15 mg/dL—hyperkalemia 5.8 mmol/L), rhabdomyolysis (CKP 3375 UI/L), and fulminant liver failure (TGO 5844 UI/L, TGP 4376 UI/L, prothrombin time 23%, factor V 17% and ammonia 194 µg/dL). A toxicological urine exam confirmed positive results for MDMA and initiated continuous renal replacement therapy with hemodiafiltration for metabolic acidosis, hyperlactatemia, and hyperammonemia. During the first 6 hours, he additionally presented critical thrombocytopenia, severe acute respiratory distress syndrome (PaO2/FiO2 ratio 67), and cardiac failure with systolic biventricular deterioration (troponin 1553 pg/mL, transesophageal echocardiogram with ejection fraction of 29%). He persisted with hypoxemia and refractory shock even though the high dose of vasopressors and inotropic administered and protective mechanical ventilation strategy; therefore, it was decided to initiate arteriovenous ECMO support. Figure 1 shows vasopressors and FiO2% requirement and the evolution of lab findings since hospital admission.
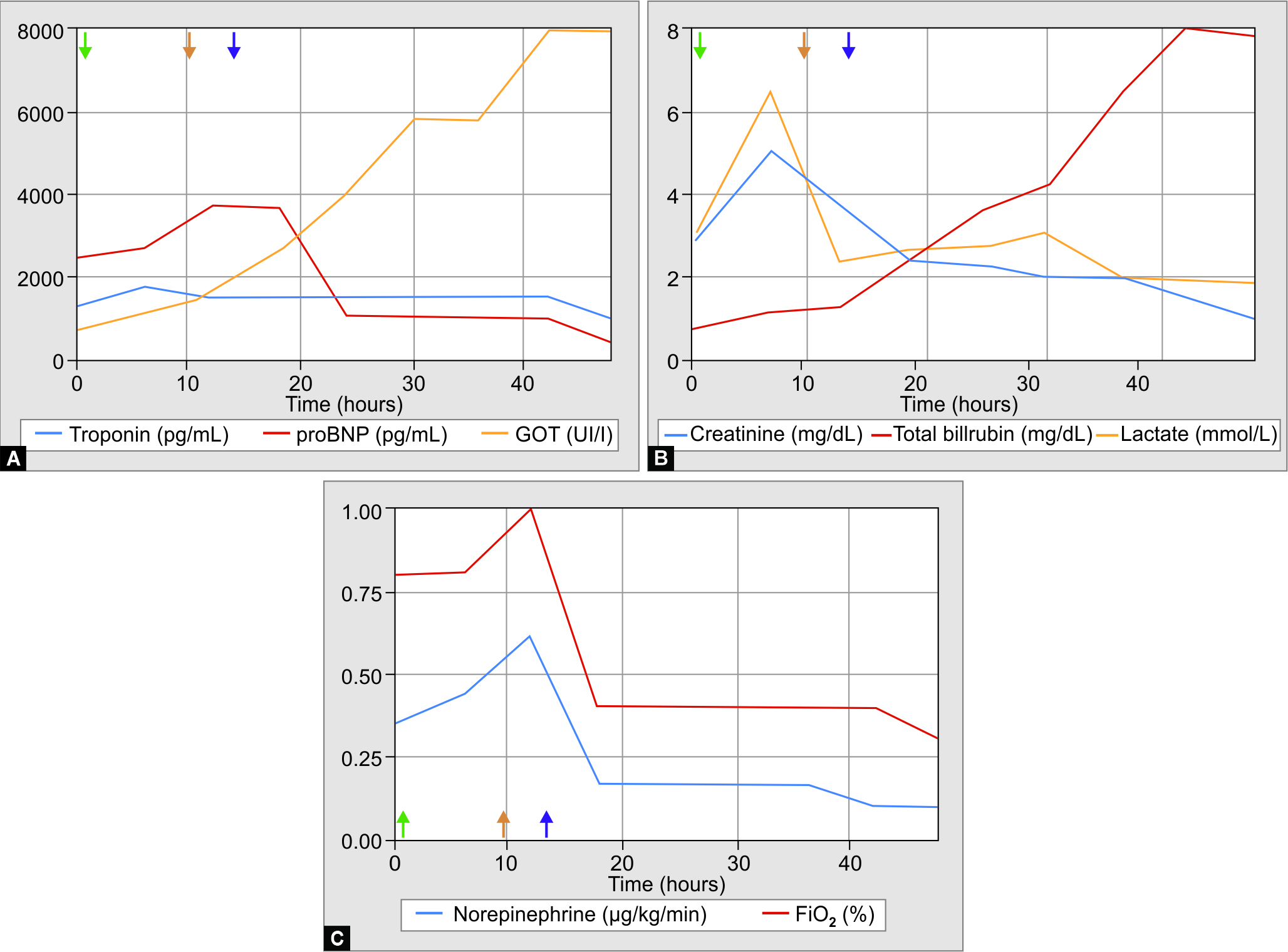
Figs 1A to C: Vasopressors and FiO2% requirement and the evolution of lab findings since hospital admission. Orotracheal intubation (green arrow), hemodialysis (orange arrow), and ECMO initiation (violet arrow). proBNP, pro B-type natriuretic peptide; FiO2, fraction of inspired oxygen; ECMO, extracorporeal membrane oxygenation
He evolved favorably with hemodynamic and respiratory improvement and a gradual decrease of vasopressors. He required extracorporeal support for 9 days, and he did not present associated complications. He was discharged after 104 days. In a 6-month period, he was able to realize everyday life activities with no sequel.
CONCLUSION
Even though there is no formal suggestion of the use of ECMO in MDMA poisoning, this report proposes to open the discussion about the recognition of this device and its use, considering the timing of its implementation fundamental in relation to its potential of future recovery. In this line, extracorporeal support could be transferable to further situations that nowadays do not possess a formal recommendation by international societies.
ORCID
Victoria Ruiz https://orcid.org/0000-0002-5138-7087
Foda Rosciani https://orcid.org/0000-0001-5402-1649
Indalecio Carboni Bisso https://orcid.org/0000-0002-4834-4676
Marcos Las Heras https://orcid.org/0000-0001-9936-0695
REFERENCES
1. Kalant H. The pharmacology and toxicology of “ecstasy” (MDMA) and related drugs. CMAJ 2001;165(7):917–928. PMID: 11599334.
2. Group CEW, Community Epidemiology Work Group. Epidemiologic trends in drug abuse: highlights and executive summary. PsycEXTRA Dataset 2001. DOI: 10.1037/e598902007-001.
3. Shannon M. Methylenedioxymethamphetamine (MDMA, “Ecstasy”). Pediatr Emerg Care 2000;16(5):377–380. DOI: 10.1097/00006565-200010000-00022.
4. Wu D, Otton SV, Inaba T, Kalow W, Sellers EM. Interactions of amphetamine analogs with human liver CYP2D6. Biochem Pharmacol 1997;53(11):1605–1612. DOI: 10.1016/s0006-2952(97)00014-2.
5. Colado MI, Williams JL, Green AR. The hyperthermic and neurotoxic effects of “Ecstasy” (MDMA) and 3,4 methylenedioxyamphetamine (MDA) in the Dark Agouti (DA) rat, a model of the CYP2D6 poor metabolizer phenotype. Br J Pharmacol 1995;115(7):1281–1289. DOI: 10.1111/j.1476-5381.1995.tb15037.x.
6. Davies N, English W, Grundlingh J. MDMA toxicity: management of acute and life-threatening presentations. Br J Nurs 2018;27(11):616–622. DOI: 10.12968/bjon.2018.27.11.616.
7. Wang GS, Levitan R, Wiegand TJ, Lowry J, Schult RF, Yin S, et al. Extracorporeal Membrane Oxygenation (ECMO) for severe toxicological exposures: review of the Toxicology Investigators Consortium (ToxIC). J Med Toxicol 2016;12(1):95–99. DOI: 10.1007/s13181-015-0486-8.
8. Attia MY, Abdelbary AA, Khaled MM, Abdelfattah AH. Veno-venous extracorporeal membrane oxygenation in a case of organophosphorus poisoning. Egypt J Crit Care Med 2016;4(1):43–46. DOI: 10.1016/j.ejccm.2016.02.006.
9. Mehra A, Sharma N. ECMO: A ray of hope for young suicide victims with acute aluminum phosphide poisoning and shock. Indian Heart J 2016;68(3):256–257. DOI: 10.1016/j.ihj.2016.02.006.
10. Bagate F, Radu C, Mekontso Dessap A, de Prost N. Early extracorporeal membrane oxygenation for cardiovascular failure in a patient with massive chloroquine poisoning. Am J Emerg Med 2017;35(2):380.e3–380.e4. DOI: 10.1016/j.ajem.2016.08.058.
11. Sutar A, Venkategowda PM, Murthy A, Chikkaswamy SB. Severe amlodipine toxicity: a case rescued with extracorporeal membrane oxygenation. Indian J Crit Care Med 2020;24(5):365–366. DOI: 10.5005/jp-journals-10071-23423.
12. Thakkar A, Parekh K, El Hachem K, Mohanraj EM. A case of MDMA-associated cerebral and pulmonary edema requiring ECMO. Case Rep Crit Care 2017;2017:6417012. DOI: 10.1155/2017/6417012.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.